Quality Improvement/Patient Safety 5
Session: Quality Improvement/Patient Safety 5
471 - Feet on the Floor: A Quality Improvement Intervention to Support Inpatients with Restrictive Eating Disorders and Decrease Time to Medical Clearance
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 471.4921
Josh Borus, Boston Children's Hospital, Auburndale, MA, United States; Kelly L.. Dunn, Boston Childrens Hospital, Jamaica Plain, MA, United States; Gabriela Vargas, Boston Children's Hospital, Boston, MA, United States; Maria G. Biancarelli, Boston Children's Hospital, Brookline, MA, United States; Elizabeth R. Woods, As an individual physician, Andover, MA, United States; Carly Guss, Boston Children's Hospital, Boston, MA, United States; Rebecca F. O'Brien, Boston Children's Hospital, Ipswich, MA, United States; Frinny Polanco, Boston Children's Hospital, Boston, MA, United States; Shannon L. Fitzgerald, Boston Childrens, Boston, MA, United States; Anthony Dekermanji, Boston Children's Hospital, Boston, MA, United States; Alexandra Healy, Boston Children’s Hospital, Washington, DC, United States; Tracy Richmond, Boston Children's Hospital, Boston, MA, United States
- JB
Josh Borus, MD, MPH
Attending Physician, Division of Adolescent/Young Adult Medicine
Boston Children's Hospital
Auburndale, Massachusetts, United States
Presenting Author(s)
Background: Bedrest initially supports medical stabilization in patients with malnutrition due to restrictive eating disorders (REDs) by reducing energy expenditure, yet prolonged bedrest may hamper recovery. Brief structured ambulation initiated earlier in hospitalization may balance energy preservation with improved vital signs and mental health.
Objective: To institute protocolized, supervised on-unit walks earlier in hospitalization for patients with REDs and assess impact on time to medical clearance for discharge.
Design/Methods: We launched the “Feet on the Floor” initiative in January 2023. Feet on the Floor was created with input from a team including medicine, nursing and nutrition. It replaced subjective criteria for ambulation with standardized clearance for supervised on-unit walks. Clearance criteria were based on vital sign stability and communicated by an electronic order. Our primary intervention consisted of education of staff and then weekly reminders from nursing to faculty and fellows to consider earlier ambulation clearance. A data collection tool asking about medical clearance was added to the billing process to expedite data capture and remind faculty. We led teaching sessions for floor nursing staff to familiarize all caregivers with the protocol. Pre-intervention data was collected by chart review of admissions from January-December 2022 to Adolescent Medicine with diagnostic billing codes of: anorexia nervosa (AN), atypical AN and OSFED, and excluded Avoidant Restrictive Food Intake Disorder. The post intervention period lasted 12 months. We evaluated length of time to medical clearance for inpatient psychiatric and residential level of care using an Xbar-S chart.
Results: The length of time to medical clearance decreased from 7.7 hospital days to 6.2 hospital days. This led to a mean shift denoting special cause variation (not due to random variation) once the intervention had been entrenched 7 months into the project and was sustained for the remainder of the tracking period. Medical Staff implementation averaged a few minutes per week. Additional benefits included qualitative increases in patient and family satisfaction, positive mood effects, and positive feedback from the nursing team.
Conclusion(s): Our simple, low-cost initiative increasing ambulation in patients hospitalized for EDs was associated with post-intervention reduction in time to medical clearance. Limitations include inability to control for patient severity. Next steps include additional measures of the intervention’s impact on mood and patient satisfaction and continuing to refine our ambulation clearance criteria.
Time From Admission To Medical Clearance for Highest Level of Care For Patients with Restrictive Eating Disorders
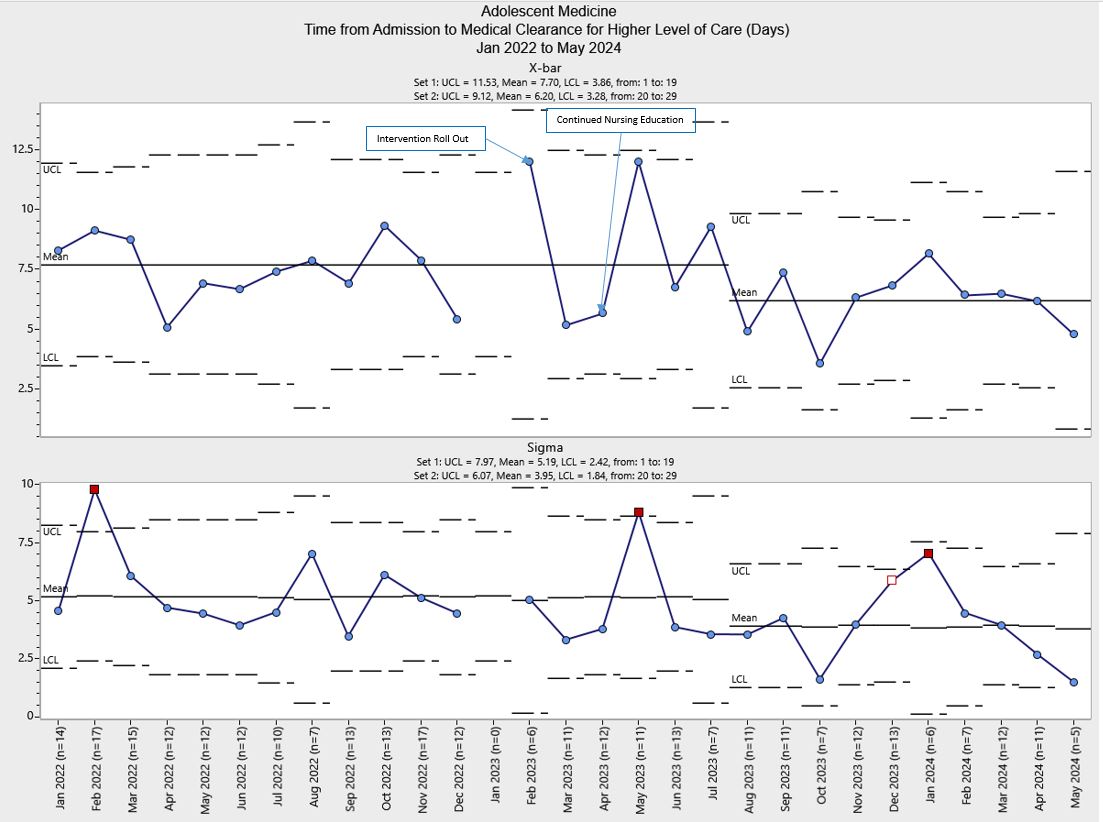 Time to medical clearance decreased by 1.5 days after full acculturation of Feet on the Floor program.
Time to medical clearance decreased by 1.5 days after full acculturation of Feet on the Floor program.

