Mental Health 2
Session: Mental Health 2
772 - Examining the Relationship Between Sociodemographic Factors and Mental Health in Childhood-Onset Systemic Lupus Erythematosus
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 772.4955
Jasmine Jing, The Hospital for Sick Children, Toronto, ON, Canada; Paris Moaf, The Hospital for Sick Children, Mississauga, ON, Canada; Lawrence Ng, SickKids, Toronto, ON, Canada; Asha Jeyanathan, The Hospital for Sick Children, Toronto, ON, Canada; Jida Jaffan, The Hospital for Sick Children, Toronto, ON, Canada; Deborah M.. Levy, The Hospital for Sick Children, Toronto, ON, Canada; Linda T.. Hiraki, The Hospital for Sick Children, Toronto, ON, Canada; Angela C. Cortes, Sick kids, Milton, ON, Canada; Eugene Cortes, SickKids, Milton, ON, Canada; Sandra Williams-Reid, TTI TRAVEL CANADA, Ajax, ON, Canada; Kiah Reid, McMaster University, Ajax, ON, Canada; Ashley Danguecan, The Hospital for Sick Children, Toronto, ON, Canada; Andrea Knight, The Hospital for Sick Children, Toronto, ON, Canada
.jpg)
Jasmine Jing (she/her/hers)
Undergraduate Volunteer Researcher
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Childhood-onset systemic lupus erythematosus (cSLE) is a chronic autoimmune disease with significant adverse impact on mental health. Furthermore, patients with cSLE often face health disparities due to marginalization involving individual-level race and ethnicity, household-level and neighborhood-level socioeconomic factors.
Objective: We aimed to understand the impact of multi-level sociodemographic factors for marginalization on mental health in youth with cSLE.
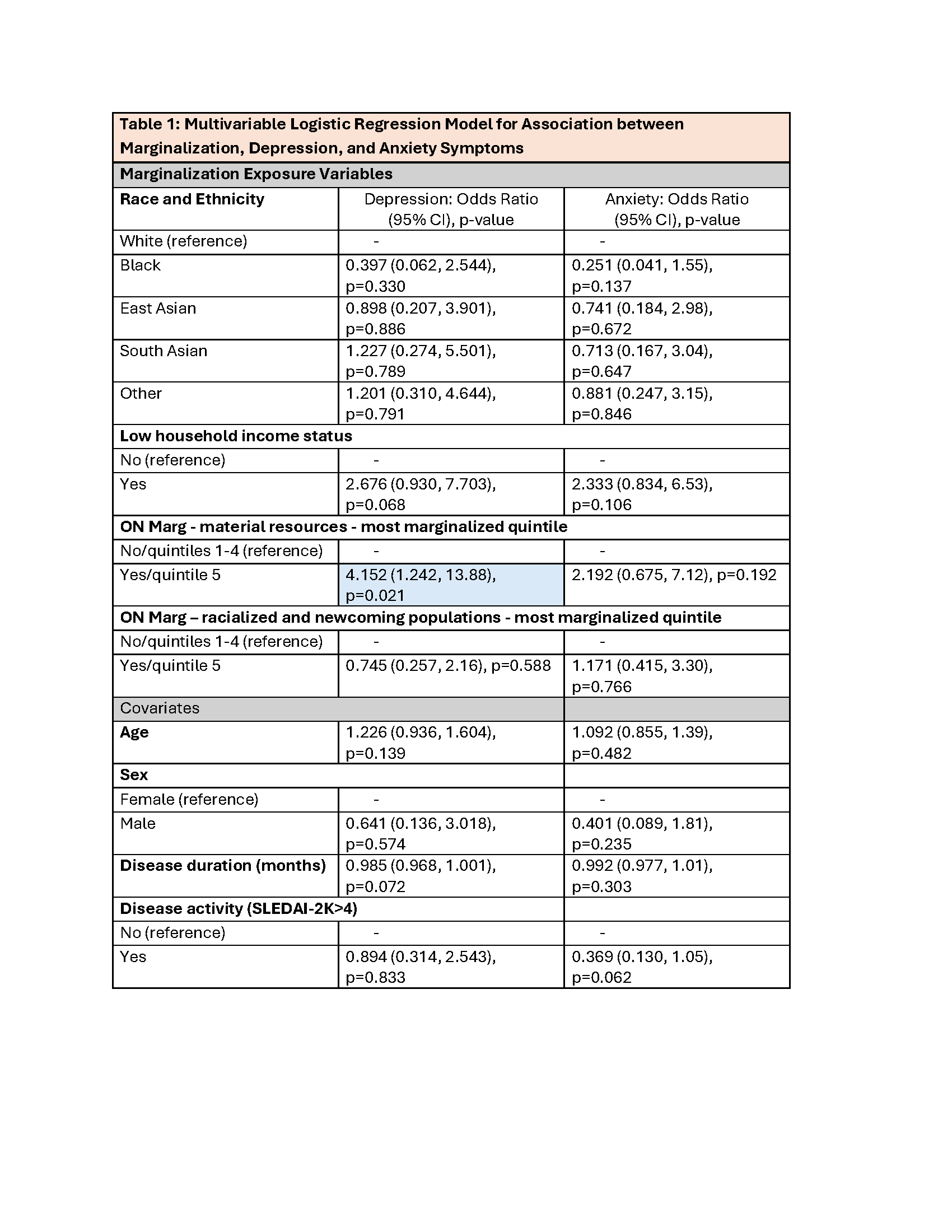
Design/Methods: We conducted a retrospective cross-sectional cohort study of publicly insured patients with cSLE (9-18 years) recruited from an outpatient lupus clinic in Ontario, Canada from October 2017-December 2023. All patients met ACR or SLICC criteria for SLE classification. The exposure of marginalization included measures for individual race and ethnicity, household low-income status, and neighborhood level Ontario Marginalization Index (material resources, racialized and newcomer population dimensions). Mental health outcomes included the presence of clinically elevated anxiety symptoms, measured by the Screen for Childhood Anxiety Related Disorders (SCARED), and depression symptoms, measured by the Center for Epidemiologic Studies Depression Scale for Children (CES-DC) or Children’s Depression Inventory/Beck Depression Inventory (CDI/BDI). Logistic regression models examined associations between the marginalization exposure variables and the mental health outcomes, adjusting for age, sex, disease duration and activity.
Results: 100 patients with cSLE were included. Marginalization characteristics are shown in Figure 1. 27% of the cohort lived in low-income households, and 52% lived in areas with the highest density of racialized and newcomer populations. Symptoms for anxiety were present in 43% and depression in 40%. Patients living in the most marginalized quintile of neighborhood material resources had higher odds of depressive symptoms compared to those in more material resourced neighborhoods (OR=4.2, 95% CI 1.2-13.9, p=0.02, Table 1). No other significant associations were observed for depressive symptoms, and no associations were found for anxiety symptoms.
Conclusion(s): In a publicly insured Canadian cohort of youth with cSLE, we found that those living in neighborhoods with the lowest material resources were at highest risk for depression symptoms. Further research into other social determinants of health is essential to improve mental health support for youth with cSLE from diverse socioeconomic backgrounds.
Figure 1
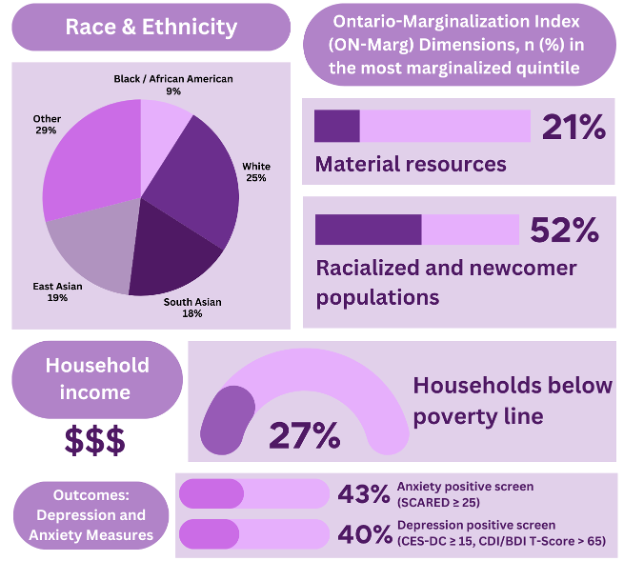 Figure 1: Shown are marginalization characteristics and mental health outcomes for the cSLE cohort (n=100).
Figure 1: Shown are marginalization characteristics and mental health outcomes for the cSLE cohort (n=100).The “Other” race and ethnic category included individuals identifying as Indigenous, Middle Eastern, Southeast Asian, or multi-ethnicity.
Table 1