Neonatal Hemodynamics and Cardiovascular Medicine 2
Session: Neonatal Hemodynamics and Cardiovascular Medicine 2
049 - Echocardiography for Detection of Pulmonary Hypertension in Infants with Severe Bronchopulmonary Dysplasia: Data from Guideline Implementation
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 49.4936
Erica McArthur, Emory University School of Medicine, Atlanta, GA, United States; Megha Kalia, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Alice Hales-Kharazmi, Emory University School of Medicine, Atlanta, GA, United States; Hui Huang, Emory University School of Medicine, Alpharetta, GA, United States; Shasha Bai, Emory University School of Medicine, Atlanta, GA, United States; Brenda Anani, Children's Healthcare of Atlanta, Atlanta, GA, United States; Anna B. Gay, Children's Healthcare of Atlanta, Dunwoody, GA, United States; Rachel McKay, Children's Healthcare of Atlanta, Atlanta, GA, United States; Shazia Bhombal, Children's Healthcare of Atlanta/Emory University, Atlanta, GA, United States; Shilpa Vyas-Read, Emory University, Atlanta, GA, United States

Shazia Bhombal, MD
Associate Professor
Children’s Healthcare of Atlanta/Emory University
Atlanta, Georgia, United States
Presenting Author(s)
Background: Pulmonary hypertension (PH) is present in ≈ 25% of infants with severe bronchopulmonary dysplasia (sBPD), and echocardiography (echo) is often utilized for its detection. In 2020, our neonatal intensive care unit (NICU) implemented risk-based echo screening, beginning as early as 32 weeks’ post-menstrual age (PMA), for PH in infants with sBPD.
Objective: To determine the proportion of infants with sBPD receiving echos and to determine echo parameters associated with PH at discharge.
Design/Methods: Infants with sBPD in our NICU (2019-2023) admitted prior to 37 weeks’ PMA had records reviewed retrospectively. Demographics/sBPD diagnoses were abstracted from the Children’s Hospitals Neonatal Consortium database. The primary outcome of discharge PH was defined by vasodilator use, clinical diagnosis, and review of the final echo report by cardiology. The proportions of sBPD infants admitted < 34 weeks’ PMA (echos at 32 +/- 2 weeks’) and < 37 weeks’ PMA (echos 36 +/- 2 weeks’ PMA) were calculated and appropriate statistical tests were utilized to evaluate differences in outcomes. Multivariable logistic models were applied to identify the echo parameters associated with PH at discharge.
Results: One-hundred and seven patients with sBPD were admitted prior to 37 weeks’ PMA, with 89 admitted prior to 34 weeks’ PMA. Sixty-six percent of patients admitted < 37 weeks’ had an echo at 36 weeks’ PMA, which stayed stable over the years of the study, while the percentage of patients receiving screening 32-week echos increased over time (Fig 1). Overall, 26% of infants had PH, and more infants with PH died or were transferred out (Table 1). On 32 weeks’ PMA echos, more infants with PH had bidirectional/right-to-left shunting through an atrial septal defect (ASD; p=0.03) and septal flattening (p=0.04) than those without PH. On 36 weeks’ PMA echo, right ventricular hypertrophy (RVH) and septal flattening were significantly different between the cohorts with and without PH (Table 1). Multivariable models controlled for gestational age showed a 11-fold and 5-fold higher odds for PH at discharge for infants with ASD or RVH on 36 weeks’ PMA echo, respectively (Table 2).
Conclusion(s): Since PH screening implementation at our site, more infants with sBPD receive echos at 32 weeks’ and ≈ 2/3 of infants receive echos at 36 weeks’ PMA. Infants with early echo changes at 32 weeks’ or ASD and RVH at 36 weeks’ have increased risk for PH at discharge. Future studies with larger sample sizes should be conducted to optimize screening and to determine early modifiable factors that may impact the risk for PH in infants with sBPD.
Figure 1. Echocardiographic screening at 32 weeks’ and 36 weeks’ PMA between 2019-2023
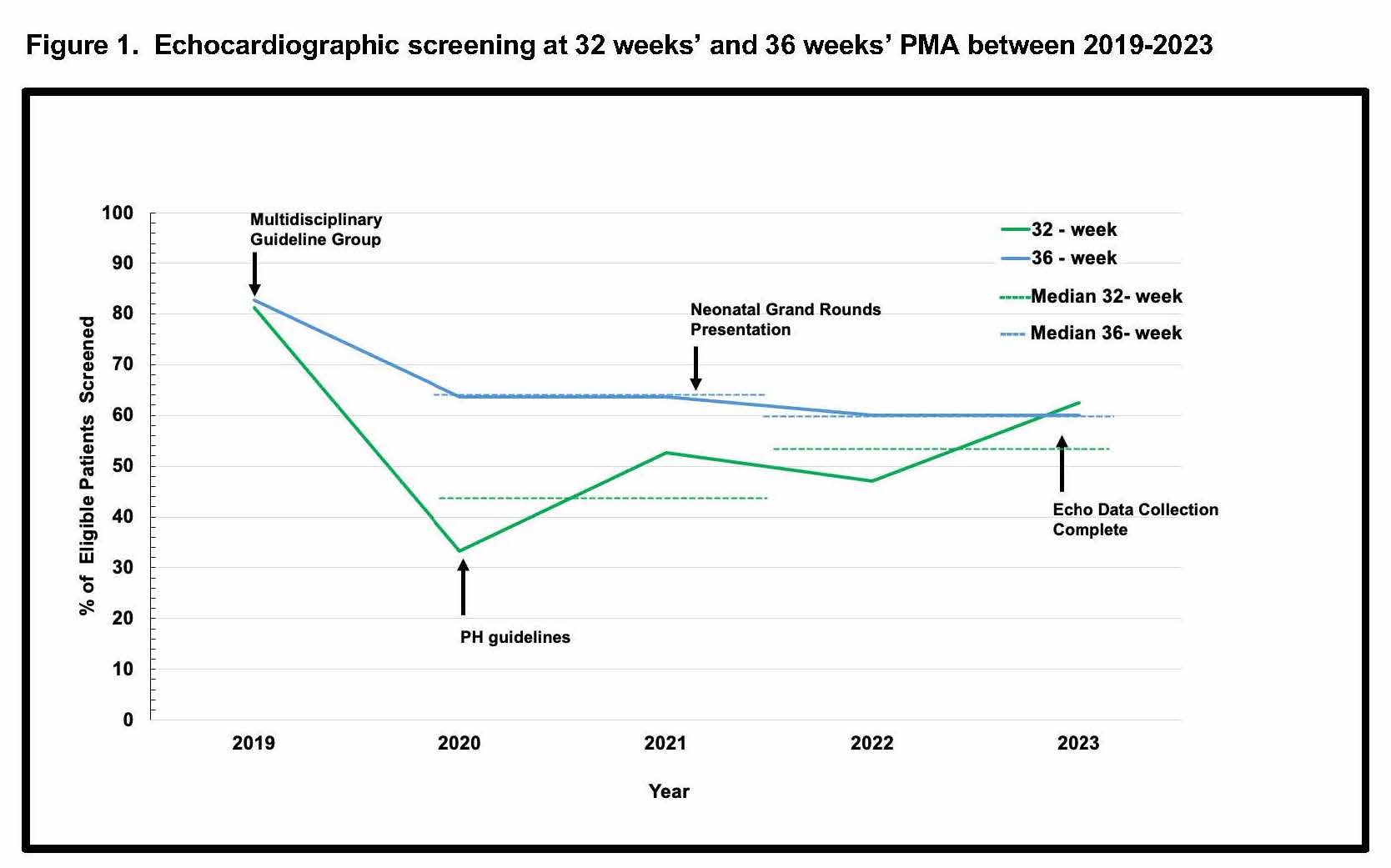 The percentage of echocardiographs performed at 32 weeks' PMA (green) and 36 weeks' PMA (blue), along with median values (dashed lines) are shown by year over the study period.
The percentage of echocardiographs performed at 32 weeks' PMA (green) and 36 weeks' PMA (blue), along with median values (dashed lines) are shown by year over the study period. Table 1. Demographics and Echocardiographic Parameters at 36 Weeks’ PMA, Overall and by PH at Discharge
.jpg) Demographic characteristics and selected echocardiographic parameters at 36 weeks' are shown. Abbreviations: LPM -- liters per minute; IMV -- Invasive mechanical ventilation; HFOV - high-frequency oscillatory ventilation; PFO -- patent foramen ovale; ASD -- atrial septal defect. Statistical tests used are shown at the bottom of the table, * p < 0.05 was significant.
Demographic characteristics and selected echocardiographic parameters at 36 weeks' are shown. Abbreviations: LPM -- liters per minute; IMV -- Invasive mechanical ventilation; HFOV - high-frequency oscillatory ventilation; PFO -- patent foramen ovale; ASD -- atrial septal defect. Statistical tests used are shown at the bottom of the table, * p < 0.05 was significant.Table 2. Logistic regression with 36 week-PMA Echocardiographic Co-variates and PH at Discharge
.jpg) Stepwise AIC, LASSO regression, and Random Forest models were applied to identify the most important predictors of PH at discharge. Shown are odds ratios, 95% confidence intervals. PFO -- patent foramen ovale; ASD -- atrial septal defect. *p < 0.05.
Stepwise AIC, LASSO regression, and Random Forest models were applied to identify the most important predictors of PH at discharge. Shown are odds ratios, 95% confidence intervals. PFO -- patent foramen ovale; ASD -- atrial septal defect. *p < 0.05.
