Medical Education 3: Simulation
Session: Medical Education 3: Simulation
207 - Implementation and Sustainability of a Novel Neonatal Resuscitation Telesimulation Program in Level I Rural Delivery Hospitals: A Qualitative Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 207.5418
Tara Palnitkar, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Leah Mallory, Barbara Bush Children’s Hospital, Portland, ME, United States; Micheline Chipman, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Mary C. Ottolini, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Allison Zanno, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Misty Melendi, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Gloria D. Sclar, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Leah Marie Seften, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States
.jpg)
Leah Marie Seften, BS (she/her/hers)
Research Navigator
The Barbara Bush Children's Hospital at Maine Medical Center
Portland, Maine, United States
Presenting Author(s)
Background: Rural hospital delivery room teams have limited exposure to neonatal resuscitation due to low birth volumes and the rarity of these clinical scenarios, making it challenging to maintain skills. To increase training opportunities, we implemented a novel, longitudinal, telesimulation (TS) program called Maine Ongoing Outreach Simulation Education Program (MOOSE), with interprofessional delivery room teams participating in their native environments. We utilized a high-fidelity newborn manikin and provided remote facilitation and debriefing support from neonatologists and simulation educators.
Objective: Our objective was to explore the implementation of MOOSE across a rural health system, including perceived benefits, challenges, and strategies for achieving long-term sustainability.
Design/Methods: We conducted 16 semi-structured interviews with the following MOOSE participants: clinical site leads from three rural hospitals (7), simulation educators and specialists (5), current and past program coordinators (3), and a neonatologist (1). Audio files were subsequently transcribed. We used the Framework Method for our thematic analysis. We present preliminary themes that emerged from our initial round of deductive and inductive coding.
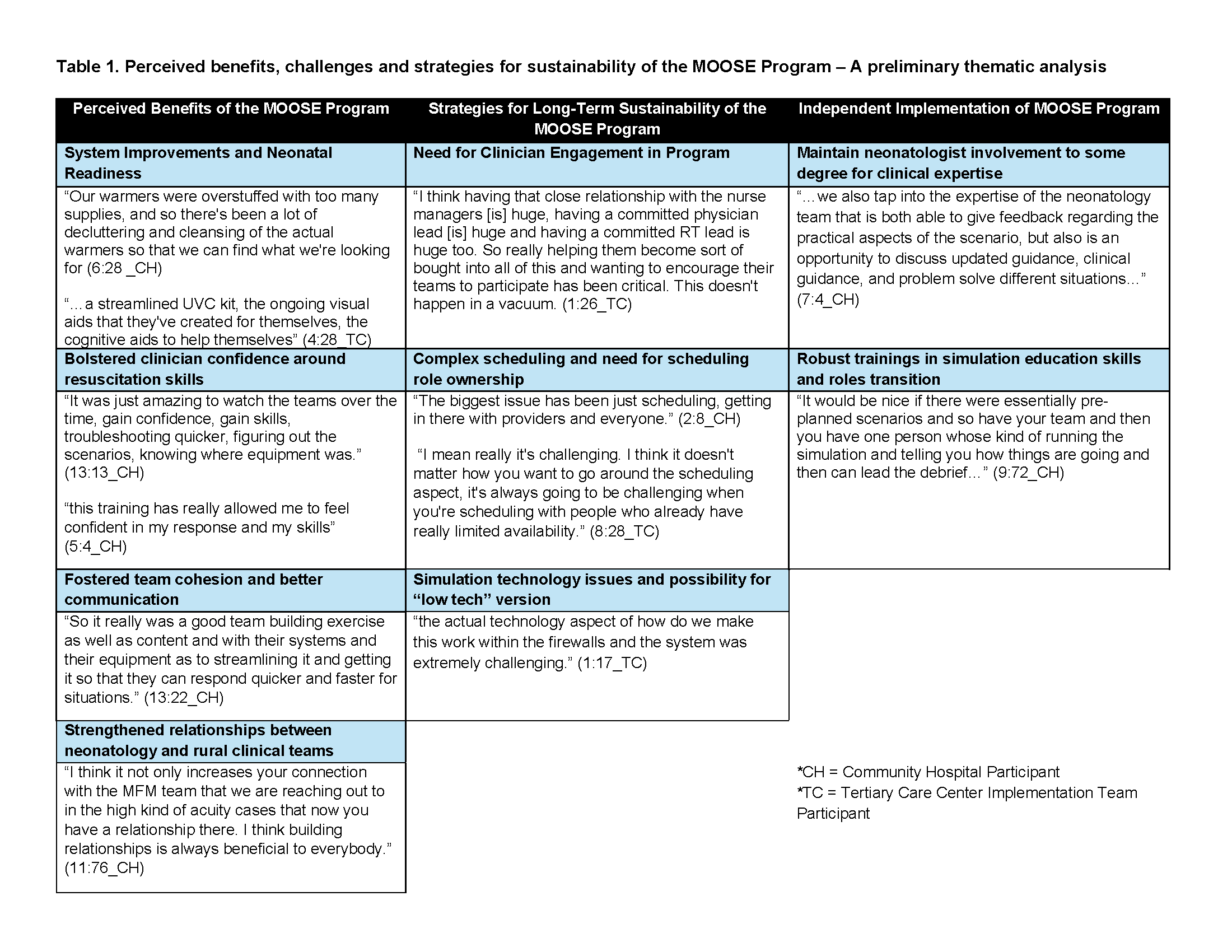
Results: Positive benefits of the program included strengthened clinical skills, system improvement for neonatal readiness, bolstered clinician confidence, better communication, and cultivated team cohesion. Participants highlighted challenges and offered recommendations, including initial resistance to attendance and a need to foster clinician buy-in. Scheduling was the most commonly noted challenge due to its complexity; a champion at each hospital who coordinates scheduling might improve ease. For long-term sustainability, participants emphasized the need to maintain neonatologist involvement to some degree because of their clinical expertise, such as an “on call” approach, and the need for simulation educators at the rural hospitals or regionally.
Conclusion(s): Longitudinal interprofessional neonatal resuscitation TS programs can positively impact neonatal readiness, clinician confidence and competence, and teamwork and procedural skills. Fostering clinician engagement, appropriate scheduling processes, access to simulation technical support and neonatology support are necessary for program improvement and sustainability. We plan to utilize recommendations to co-create a toolkit for sustainability with rural hospital leadership.
Perceived benefits, challenges and strategies for sustainability of the MOOSE Program – A preliminary thematic analysis