Hospital Medicine 1: Quality Improvement
Session: Hospital Medicine 1: Quality Improvement
552 - Improving Documentation of Overnight Changes in Clinical Status for Children Admitted to the Pediatric Hospital Medicine Service
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 552.5448
Ann Kennon. Ulicny, Children's of Alabama, Birmingham, AL, United States; Nichole Samuy, University of Alabama School of Medicine, Birmingham, AL, United States; Erin Shaughnessy, University of Alabama School of Medicine, Birmingham, AL, United States; Paul Scalici, University of Alabama School of Medicine/Children's of Alabama, Birmingham, AL, United States; Anthony Zanni, University of Alabama School of Medicine, Hoover, AL, United States; Caroline Lambert, Childrens of Alabama, Birmingham, AL, United States; Sarah Prickett, University of Alabama School of Medicine, Birmingham, AL, United States; Andrea Kennedy, University of Alabama School of Medicine, Birmingham, AL, United States; Adolfo L. Molina, UAB/Children's of Alabama, Hoover, AL, United States
- AU
Ann Kennon Ulicny, DO (she/her/hers)
Pediatric Hospital Medicine Fellow
UAB Pediatrics/Children's of Alabama
Birmingham, Alabama, United States
Presenting Author(s)
Background: Preventable adverse events are associated with “cross-coverage,” or care by another physician when the primary team is absent. Cross-coverage has increased following ACGME duty hour restrictions. A multisite study found that the primary intern is only available for 39% of the inpatient stay, necessitating frequent care transitions. The Joint Commission found that 80% of serious medical errors are related to miscommunication during patient handoff. At our institution, there are frequent anecdotal reports of significant intervention occurring overnight without related documentation, leading to incomplete understanding of the cross-cover team’s clinical reasoning.
Objective: This project aimed to improve handoff communication by increasing the documentation rate of overnight changes in clinical status by 20%, from 52% to 66%, by January 2025.
Design/Methods: A multidisciplinary team designed a quality improvement (QI) project using the Institute for Healthcare Improvement (IHI) Model for Improvement methodology. To identify patient events, five conditions were identified as a proxy for changes in clinical status warranting documentation: 1) escalation of care transfer, 2) rapid response, 3) PICU consult, 4) positive blood culture or 5) urgent CT scan. The presence of a related update note served as the primary outcome measure. Baseline data was obtained by retrospective EPIC query reports for the year prior to project initiation, showing a documentation rate of 52% for the identified events. PDSA cycles included 1) Development of standard expectations for cross-cover documentation based on literature review and internal division consensus, 2) Resident education on the role of communication failure in adverse events and 3) Addition of update note templates on the mobile EMR application to allow for documentation by phone, including dictation. Statistical process control charts were created with QI Macros for Excel to track data over time, using IHI rules for special cause variation and mean shifts. Process measures to assess workload and acuity included the total number of admissions overnight and the number of change-in-status events per month. Tracking residents staying past their allotted shift time due to increased documentation burden served as a balancing measure.
Results: The SMART aim was successfully met, with a mean shift from 52% to 66% by November 2024.
Conclusion(s): Improved documentation by the cross-cover team improves handoff communication. Since communication failure is a leading cause of medical error, this has the potential to decrease adverse events for hospitalized pediatric patients.
p-Chart Demonstrating Percentage of Events with a Documented Update Note Over Time
.png) This p-Chart shows a mean shift from 52% to 66.3% (a 27.5% increase) in the percentage of change in clinical status events with a documented patient update note.
This p-Chart shows a mean shift from 52% to 66.3% (a 27.5% increase) in the percentage of change in clinical status events with a documented patient update note. Key Driver Diagram
.png) This key driver diagram highlights that competing priorities, lack of clear guidelines surrounding documentation expectations, perception that verbal handoff is adequate and fear of adding to tension between providers are key barriers to documentation of patient update notes. By eliciting this information through brainstorming sessions, the team was able to develop targeted interventions to reach our SMART aim.
This key driver diagram highlights that competing priorities, lack of clear guidelines surrounding documentation expectations, perception that verbal handoff is adequate and fear of adding to tension between providers are key barriers to documentation of patient update notes. By eliciting this information through brainstorming sessions, the team was able to develop targeted interventions to reach our SMART aim. Pareto Chart: Events Lacking a Patient Update Note by Type of Event
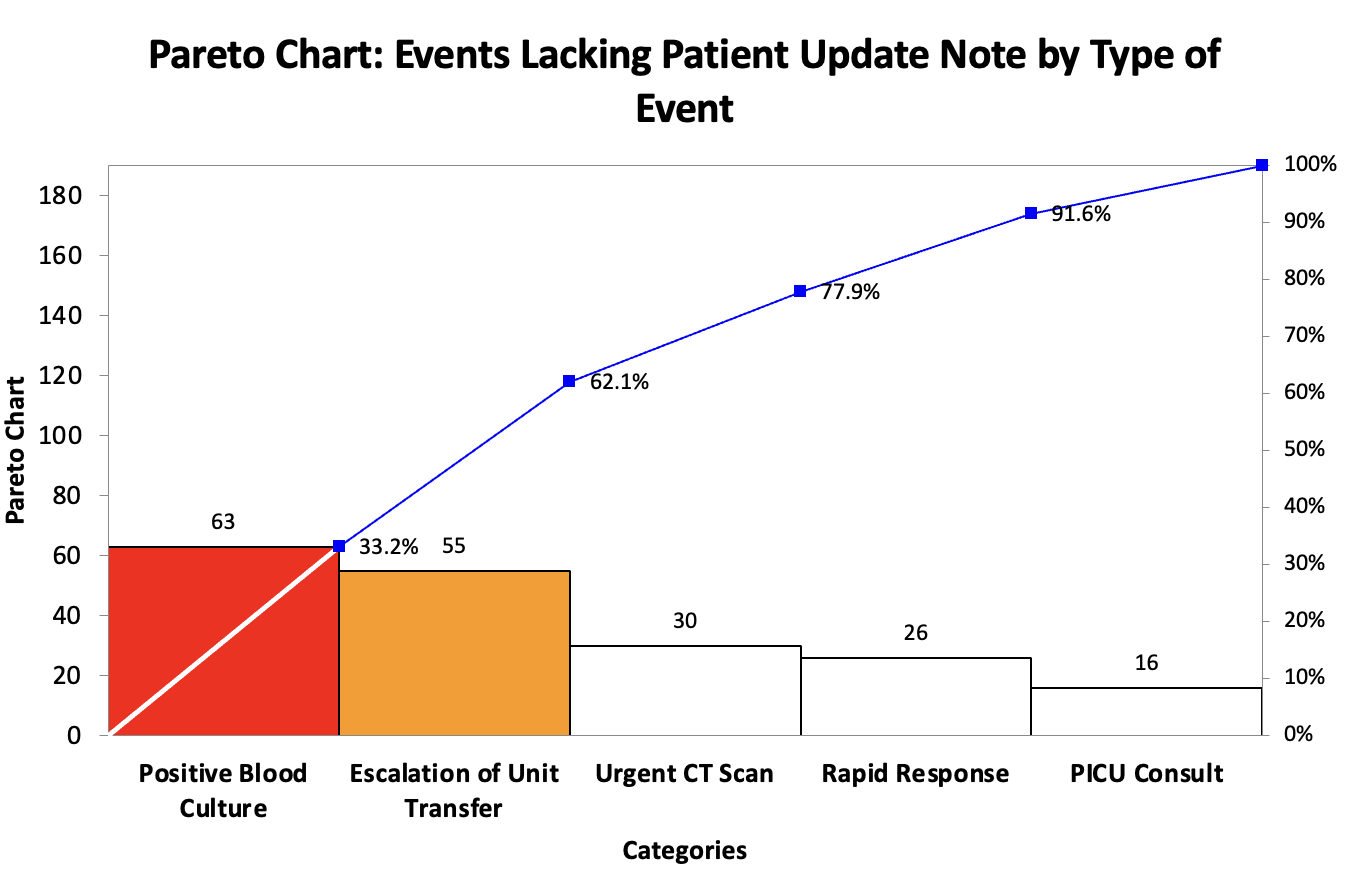 This pareto chart reveals that the most frequent events lacking a patient update note are the occurrence of a positive blood culture and an escalation of unit transfer.
This pareto chart reveals that the most frequent events lacking a patient update note are the occurrence of a positive blood culture and an escalation of unit transfer.

