Neonatal Quality Improvement 6
Session: Neonatal Quality Improvement 6
533 - Impact of Unplanned Extubation Reduction Strategies on Respiratory Outcomes and Radiation Exposure in the Neonatal ICU
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 533.5468
Amanda T. Minga, University of South Alabama Children's and Women's Hospital, Mobile, AL, United States; jeremy Norman, University of South Alabama College of Medicine, Mobile, AL, United States; Andrew Jay, USA Health Children's and Women's Hospital, Mobile, AL, United States; Brooke Olson, USA Health Childrens and Womens Hospital, Mobile, AL, United States; Manimaran Ramani, University of Alabama School of Medicine, Mobile, AL, United States; Kelechi Ikeri, University of South Alabama College of Medicine, Mobile, AL, United States

Amanda T. Minga, DNP, NNP-BC
Neonatal Nurse Practitioner
University of South Alabama Children's and Women's Hospital
Mobile, Alabama, United States
Presenting Author(s)
Background: Targeted care bundles reduce unplanned extubations (UEs). However, they may unintentionally extend the duration of mechanical ventilation (MV) in infants who do not need re-intubation after a UE. Also, maintaining optimal endotracheal tube (ET) depth requires multiple ET repositioning attempts and repeated radiologic assessments which could increase radiation exposure.
Objective: To reduce the UE rate in the NICU by 20% by July 2024. To assess MV duration, bronchopulmonary dysplasia (BPD) rates and radiation exposure.
Design/Methods: This quality improvement (QI) initiative was carried out in a 98-bed level III NICU using the Plan-Do-Study-Act model for improvement. The baseline period spanned from June to November 2023. Analysis of Apparent Cause Analysis (ACA) revealed suboptimal endotracheal tube (ET) positioning, loose ET securement methods, and malposition during repositioning as causes of UEs. Key drivers were identified, and a care bundle was implemented starting in December 2023. The bundle included standardizing the anatomic ET reference point and securement methods, assigning a dedicated staff to hold the ET during repositioning, enhancing the bedside RN hand-off process, and providing staff education. Outcome measure was the UE rate. Process measures were compliance with anatomic ET positioning and staff charting. Balancing measures were MV duration, BPD incidence ( < 33weeks GA infants), and radiation exposure.
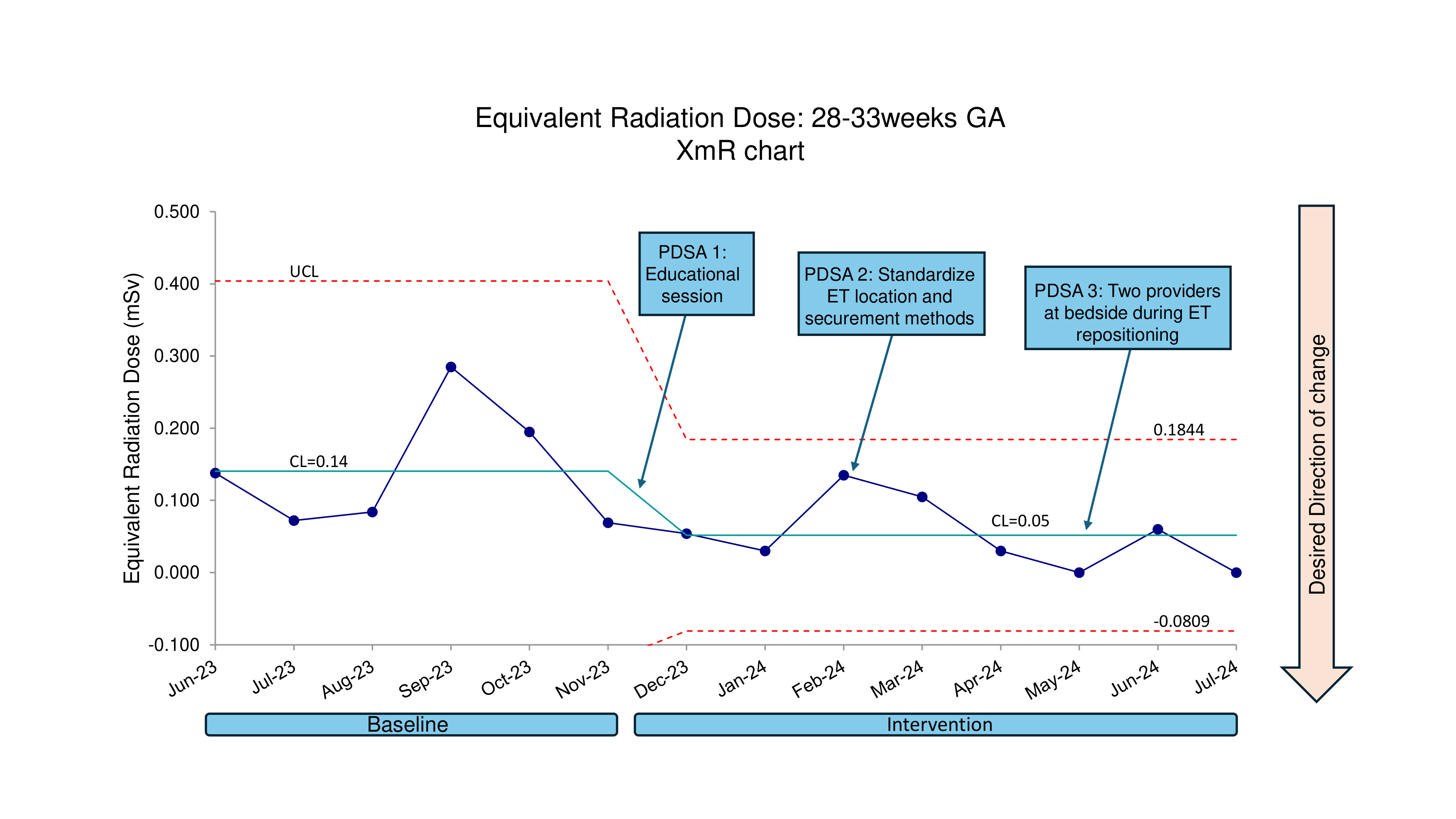
Results: A total of 151 intubated newborns were included. With intervention, UE rates were reduced from 3.3 to 1.7 per 100 ventilator days (48.4% decrease), with special cause variation (Fig1). Average monthly ventilator days per intubated infant 22-276/7 weeks GA increased from 8.4 to 10.4 days (fig. 2) with special cause variation but remained stable at 3.2 days among infants 28-326/7 weeks GA. Pre- and post-implementation BPD rates among intubated infants were 77% vs. 85% (p=0.4) for infants 22-276/7 weeks GA and 31% vs 65% (p=0.055) for infants 28-326/7 weeks GA. Average monthly equivalent radiation dose per intubated infant 22-276/7 weeks GA was stable at 0.34mSv. For infants 28-326/7 weeks GA radiation dose reduced from 0.14mSv to 0.05mSv (64% decrease) with special cause variation (fig.3).
Conclusion(s): MV duration was increased among infants < 28 weeks GA, though BPD was not worsened with UE reduction. Radiation exposure decreased among newborns 28-32 6/7 weeks GA. UE strategies may reduce radiation exposure possibly from improved ET stability with optimal positioning, which could result in fewer cardiopulmonary events warranting imaging.
Fig 1. U chart. Rate of Unplanned extubations
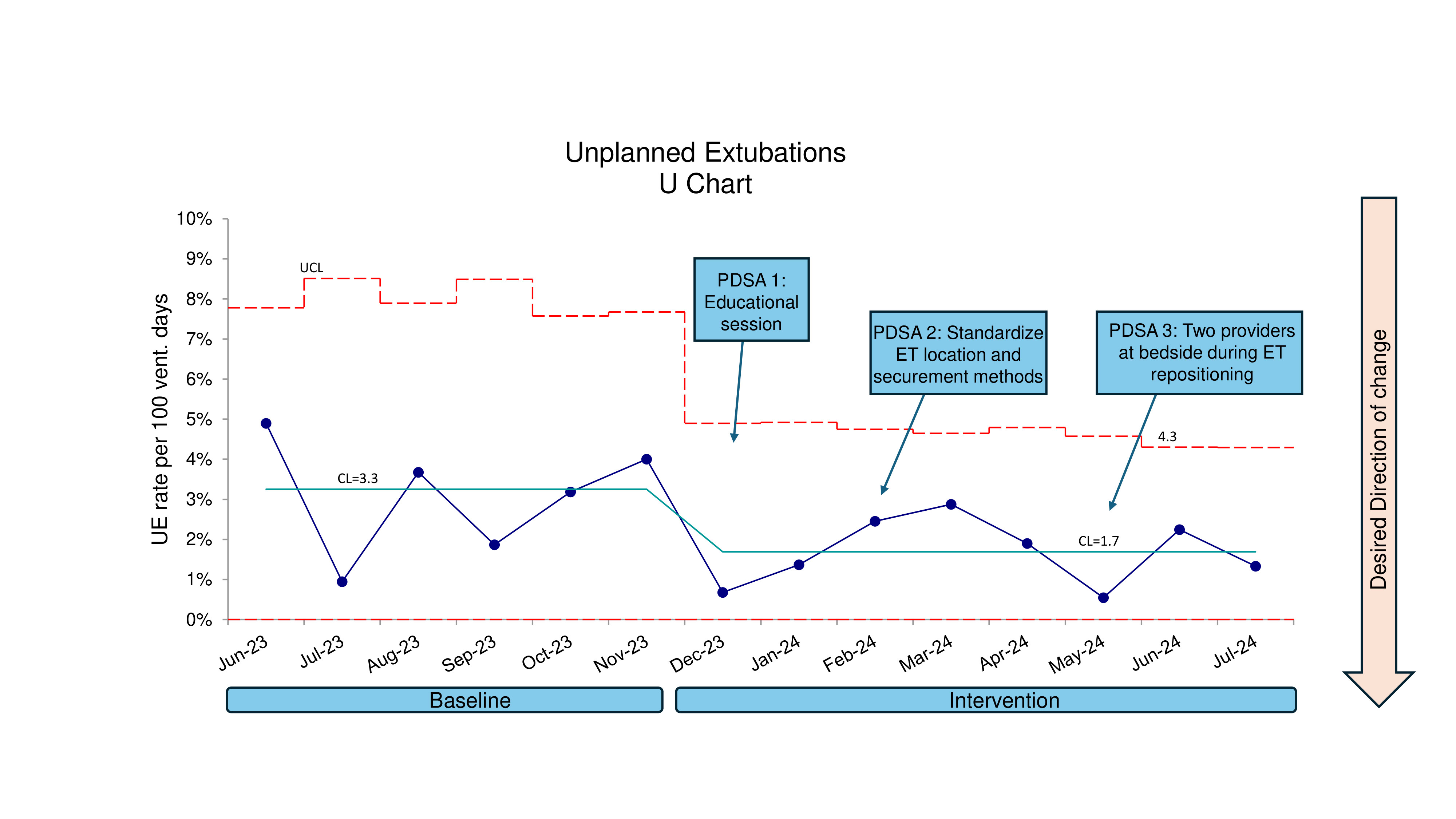
Fig 2. XmR chart. Ventilator days in infants less than 28weeks GA
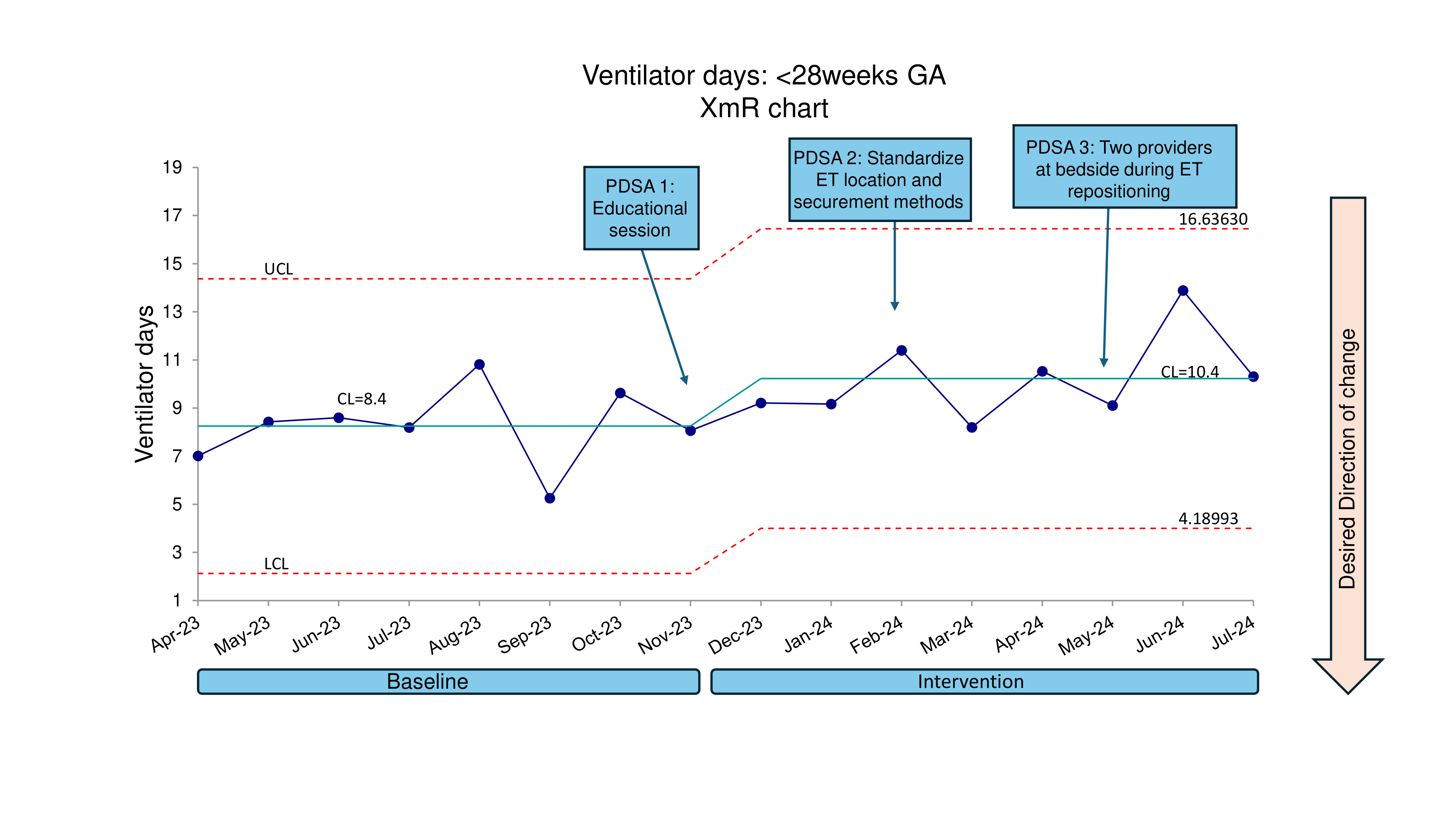
Fig 3. XmR chart. Equivalent radiation dose in 28-33week GA