Quality Improvement/Patient Safety 6
Session: Quality Improvement/Patient Safety 6
490 - Increasing Resident Involvement in Medical Resuscitation in the Pediatric Emergency Department
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 490.5410
Melissa Blumberg, Nemours Children's Hospital, Audubon, NJ, United States; Theresa C. Barrett, NemoursAlfred I. duPont Hospital for Children, Wilmington, DE, United States; Joshua Rice, Nemours Children's Hospital, Wilmington, DE, United States; Courtney Nelson, Nemours Children's Hospital, Wilmington, DE, United States
Melissa Blumberg, MD (she/her/hers)
Fellow
Nemours Children's Hospital
Audubon, New Jersey, United States
Presenting Author(s)
Background: Resident physician learners spend a limited time during their training in the Pediatric Emergency Department (PED); however, the PED provides a prime opportunity for residents to gain experience managing a critically ill child.
Objective: Our aim was to raise resident involvement in medical resuscitations (MRs) from 46% to 70% over 6 months, while also evaluating how this involvement affects their confidence in assessing and managing critically ill patients.
Design/Methods: A multidisciplinary team identified three main drivers: awareness that a MR is in progress, development of an actionable and disruptive alert system, and resident familiarity with MR roles (Fig 1). We developed a two-tier intervention using an alarm-based alert system to boost MR awareness and designated a resident per shift to prioritize MRs. MRs were defined as cases roomed in one of two resuscitation bays, excluding traumas due to separate protocols and response teams. Assigned residents were expected to rapidly respond to MRs and to engage in roles including: primary/secondary survey, order placement, history taking, note writing, and procedures. Our primary outcome measure was percentage of notes completed by residents per 25 MRs. Our process measure was use of the alarm-based alert system, which was simultaneously tracked per 25 MRs. Voluntary pre- and post-intervention surveys anonymously assessed residents’ comfort in common MR scenarios.The baseline period was July 2023 – mid-January 2024, with implementation phase from mid-January – September 2024. Three PDSA cycles each targeted different care groups to address process failure: 1) feedback to nursing on appropriate MR designation to address alert fatigue, 2) feedback to physician-assistants emphasizing their role in resident support, and 3) feedback to fellows emphasizing their role in resident teaching. We used descriptive statistics to analyze survey results and a Statistical Process Control “P” chart to analyze our process and outcome measures.
Results: Resident MR involvement rose from 46% to 68% during implementation (Fig 2), and alert usage increased from 0% to 37% (Fig 3). Pre- and post-survey trends indicated an increase in residents’ comfort across all MR scenarios post-implementation.
Conclusion(s): Standardizing MR involvement processes can enhance resident participation in MRs in the PED, potentially improving their confidence in managing critically ill pediatric patients.
Figure 1. Key Driver Diagram
.png) The key driver diagram depicts drivers and change ideas affecting our primary aim.
The key driver diagram depicts drivers and change ideas affecting our primary aim. Figure 2. Outcome Measure Control Chart
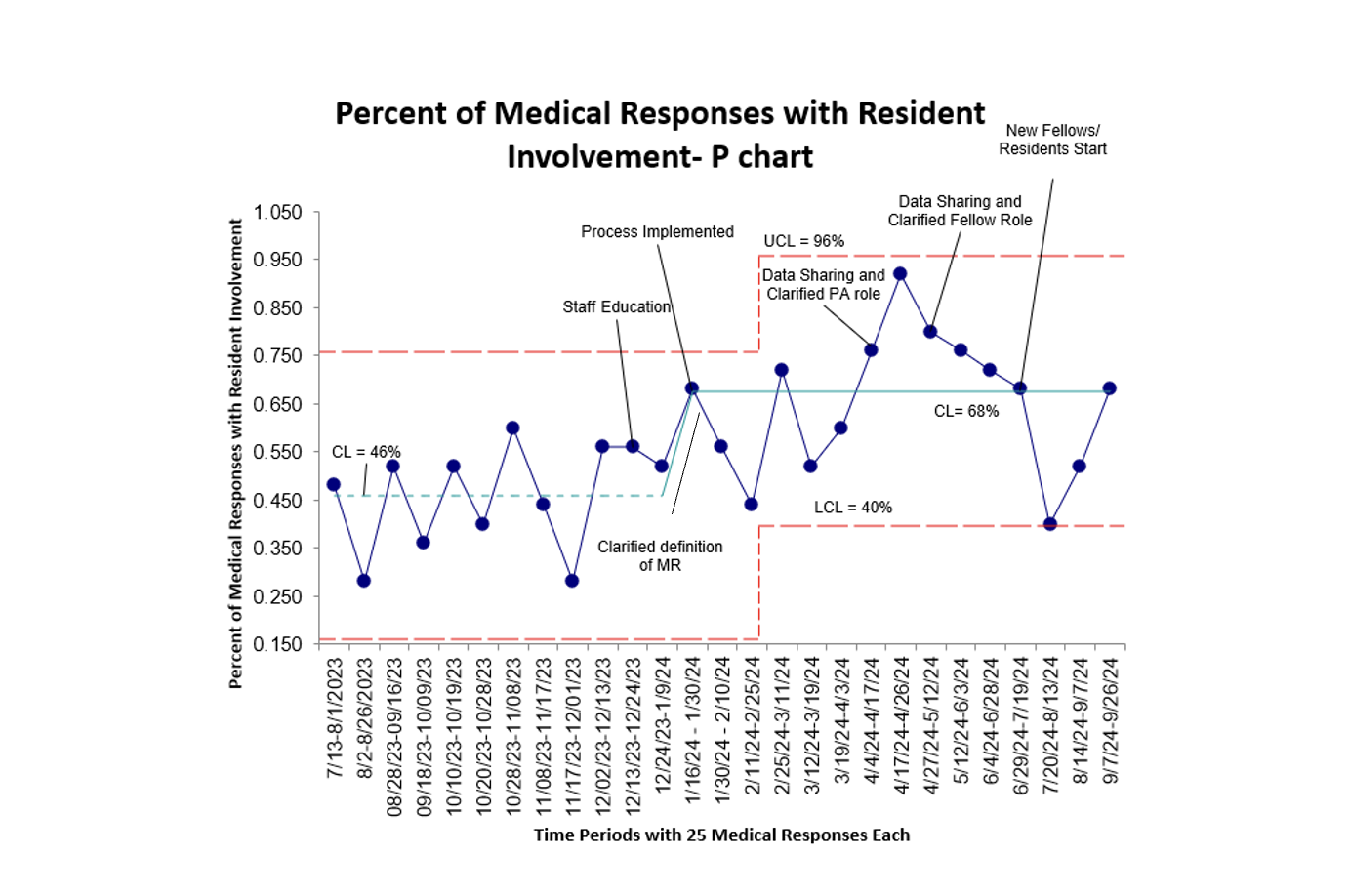 This chart depicts the percent of medical responses with resident involvement over time. Each time period represents 25 individual medical responses.
This chart depicts the percent of medical responses with resident involvement over time. Each time period represents 25 individual medical responses.Figure 3. Process Measures Control Chart
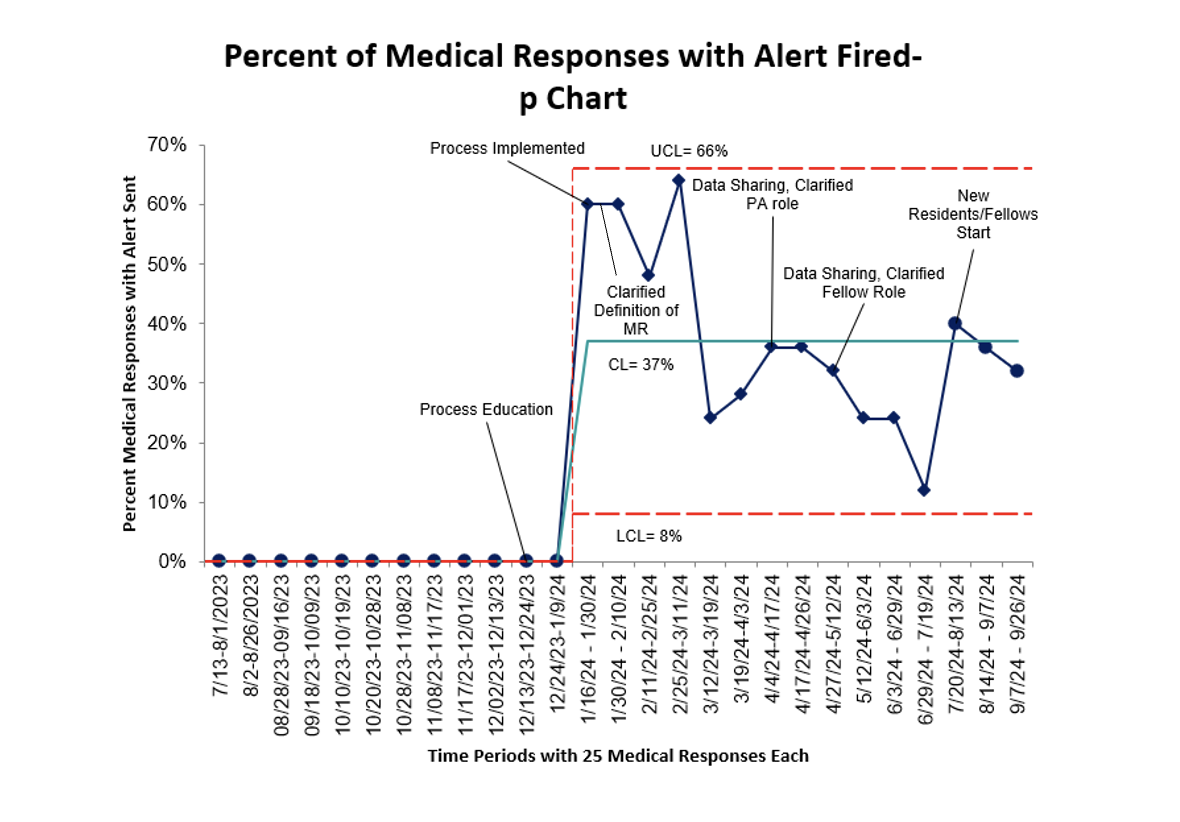 This chart depicts the percent of medical responses with an alert fired over time. Each time period represents 25 individual medical responses.
This chart depicts the percent of medical responses with an alert fired over time. Each time period represents 25 individual medical responses.

