Neonatal Quality Improvement 4
Session: Neonatal Quality Improvement 4
504 - Improving Delivery Room Efficiency for Infants with Congenital Diaphragmatic Hernia
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 504.5397
Andrew M.. Barr, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Patrick Smith, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Beth C. Haberman, Cincinnati Children's Hospital Medical Center, CINCINNATI, OH, United States; Stefanie Riddle, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Thomas Nienaber, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Nicole Comley, Cincinnati Children's Hospital Medical Center, Lebanon, OH, United States; Paul S. Kingma, Cincinnati Children's Hospital, Cincinnati, OH, United States; Morgan E. Hill, Cincinnati Children's Hospital Medical Center, Loveland, OH, United States

Andrew M. Barr, MD, MSE (he/him/his)
Clinical Fellow: Neonatal-Perinatal Medicine
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Infants with congenital diaphragmatic hernia (CDH) are at high risk for significant morbidity and mortality. Supporting an infant with CDH requires well-coordinated, efficient multidisciplinary care from the moment of birth. The Children’s National Consortium Database reports that the national median survival to discharge in CDH infants is 79.7% (2018-2024); median survival at our institution is 70%. We developed a QI initiative to increase median survival to discharge in CDH infants from 70% to 85% in 24 months (August 2025). As the use of the Neonatal Resuscitation Program (NRP) has aided in decreased neonatal mortality since its development in 1987, we similarly identified consistent and efficient delivery room practices as a key driver for this global aim (Figure 1).
Objective: This QI initiative aimed to decrease time to complete delivery room resuscitations of infants with CDH from 16.8 minutes to 10 minutes by August 1, 2025 (24 months).
Design/Methods: All infants with CDH born at our institution were targeted by this initiative. A key driver diagram was developed (Figure 1) and PDSA cycles were performed focusing on the development and implementation of standardized delivery room protocols. Time from arrival to infant warmer bed to the final step of the protocol (IV access) was assessed as a process measure marking efficiency. This process measure and adherence to the protocol were monitored through video review of each eligible resuscitation by a trained physician (AB).
Results: No standardized delivery room practice for infants with CDH was previously followed for baseline comparison. Data collection commenced after the introduction of standardized delivery room protocols for infants with CDH. Starting August 2023, 15 infants with CDH were delivered with eligible video recordings for review. Initial time to complete delivery room resuscitation using standardized protocols was 16.8 minutes. By February 2024, shift was achieved and time to complete resuscitation decreased by 55.5% to 7.5 minutes (Figure 2).
Conclusion(s): This QI initiative focused on efficient delivery room resuscitation of infants with CDH. Implementation and distribution of a standardized delivery room protocol, development of a video review program, and regular team meetings as interventions led to a successful decrease in time to complete resuscitations. Through this work and additional standardized strategies pre- and post-repair, our CDH team has shown initial improvement in survival to discharge of CDH infants and is hopeful to achieve our global aim of increasing median survival from 70% to 85% by August 2025 (Figure 3).
Figure 1. Congenital Diaphragmatic Hernia Quality Improvement Initiative Key Driver Diagrams
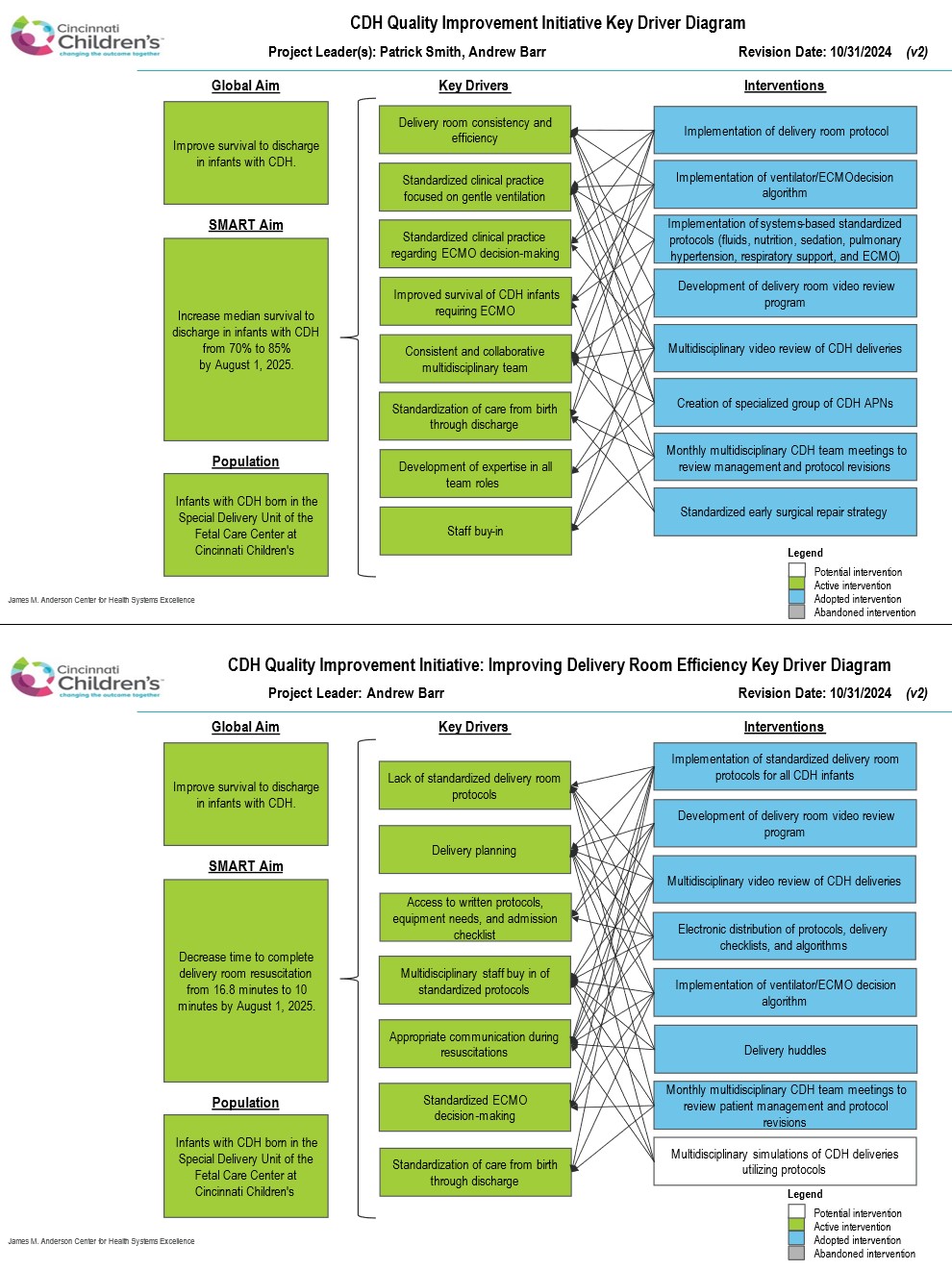 Key driver diagram for the global quality improvement initiative aimed at improving CDH survival (top) and the key driver diagram for improving delivery room consistency and efficiency (bottom), a key driver of our global aim.
Key driver diagram for the global quality improvement initiative aimed at improving CDH survival (top) and the key driver diagram for improving delivery room consistency and efficiency (bottom), a key driver of our global aim.Figure 2. CDH Delivery Room Efficiency Run Chart
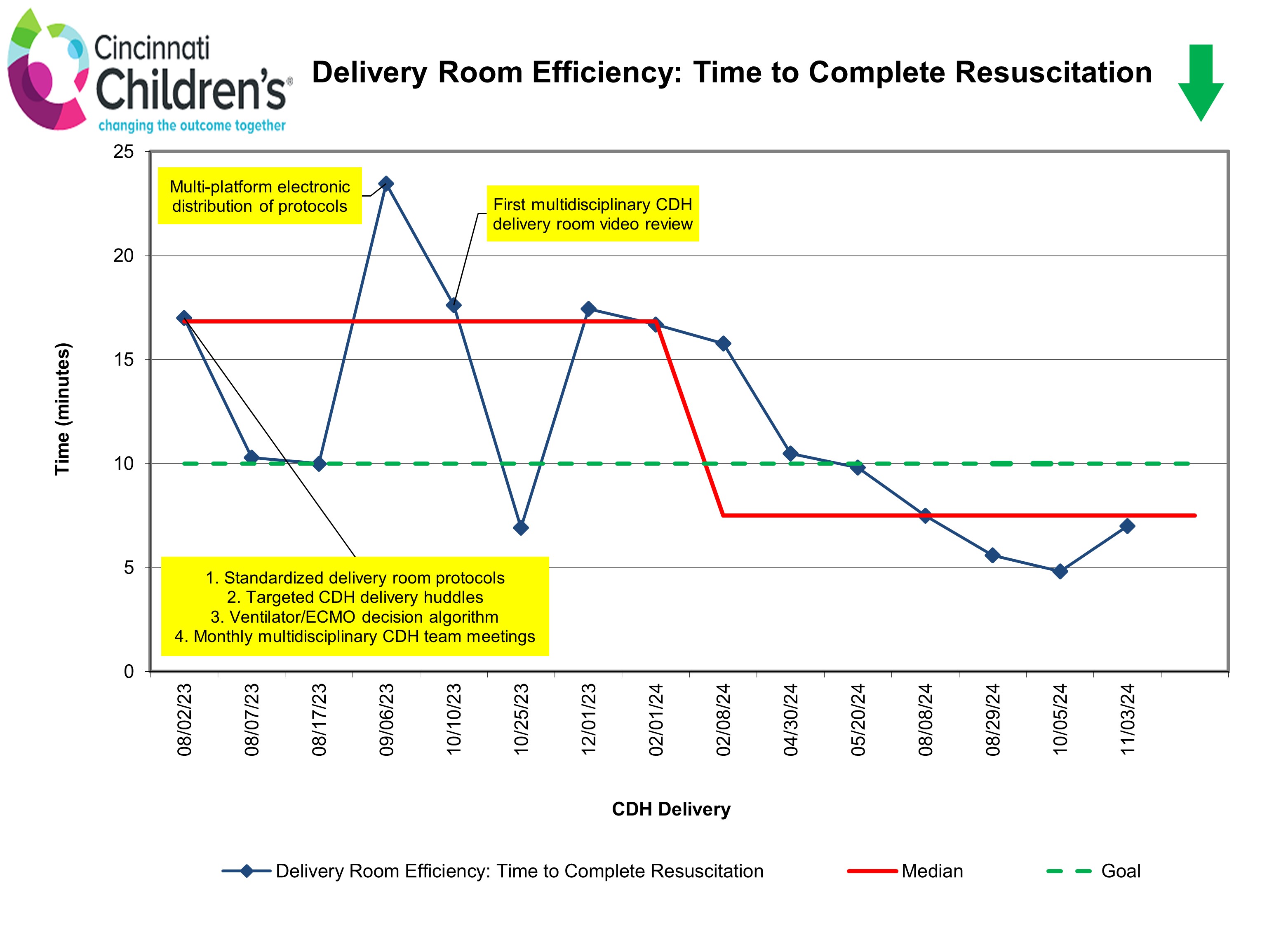 Run chart for time to complete delivery room resuscitation for CDH infants utilizing standardized protocols, defined as the time from arrival to infant warmer bed to completion of the final step of the protocol (IV access), assessed as a process measure marking efficiency. After implementation of standardized protocols and additional interventions as noted, median time to complete resuscitation decreased from a baseline of 16.8 minutes by 55.5% to 7.5 minutes.
Run chart for time to complete delivery room resuscitation for CDH infants utilizing standardized protocols, defined as the time from arrival to infant warmer bed to completion of the final step of the protocol (IV access), assessed as a process measure marking efficiency. After implementation of standardized protocols and additional interventions as noted, median time to complete resuscitation decreased from a baseline of 16.8 minutes by 55.5% to 7.5 minutes.Figure 3. Infants With CDH Who Survive to Discharge Run Chart
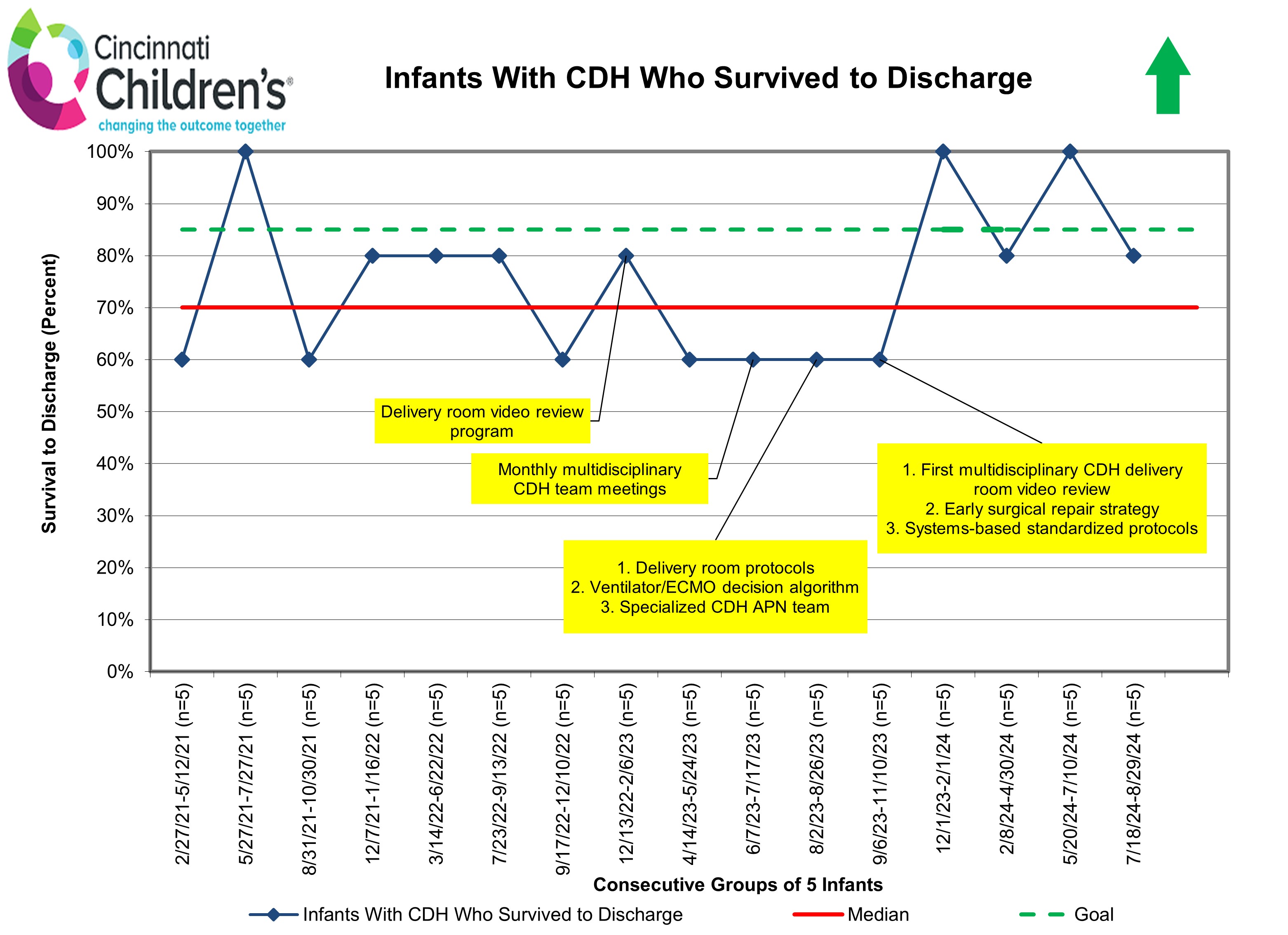 Run chart for survival to discharge of infants with CDH organized in consecutive groups of 5 infants. This shows promising initial improvement in survival to discharge through our QI initiative, and we are hopeful to achieve our global aim of increasing median survival from 70% to 85% by August 2025.
Run chart for survival to discharge of infants with CDH organized in consecutive groups of 5 infants. This shows promising initial improvement in survival to discharge through our QI initiative, and we are hopeful to achieve our global aim of increasing median survival from 70% to 85% by August 2025.

