Neonatal Quality Improvement 4
Session: Neonatal Quality Improvement 4
505 - Improving Immunization Timeliness in the Boston Children’s Hospital Neonatal Intensive Care Unit
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 505.5363
Oludare A. Odumade, University of Minnesota Medical School, Minneapolis, MN, United States; Kristen T. Leeman, Boston Children's Hospital, Boston, MA, United States; Jenna Katz, Harvard Medical School, Boston, MA, United States; Maria G. Biancarelli, Boston Children's Hospital, Brookline, MA, United States; Stacie Haralambous, Boston Children’s Hospital, Boston, MA, United States; Romane Jones, Boston Children's Hospital, Boston, MA, United States; Sandra C. Hennessy, Boston Children's Hospital, Boston, MA, United States; Julie Briere, Boston Children's Hospital, chelmsford, MA, United States; Ashley Doherty, Boston Children's Hospital, Malden, MA, United States

Oludare A. A. Odumade, MD PhD
Assistant Professor
University of Minnesota Medical School
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: Neonatal morbidity and mortality from vaccine preventable diseases remain a significant global health burden. The American Academy of Pediatrics (AAP) recommends hepatitis B vaccination within the first month and other routine vaccinations starting at two months of age for all stable newborns. However, infants admitted to the neonatal intensive care unit (NICU) are often un- or under-immunized.
Objective: To improve the percentage of eligible infants, in the level III/IV Boston Children’s Hospital (BCH) NICU, who are up to date with vaccinations at time of discharge/transfer from a current mean of 65% to ≥80% over the course of 6 months.
Design/Methods: We conducted a survey of stakeholders during Phase 1 (December 2022) to identify barriers to on-time vaccination and then outlined drivers to success on a key driver diagram (Fig. 1). PDSA cycles included (1) weekly review of vaccination status during medical rounds, increasing visibility and awareness with (2) use of tracking stickers on the rounding folders, and (3) weekly pharmacy audit and email to the NICU team. Our outcome measures were 1) percent of infants up-to-date (UTD) with vaccines on weekly chart audit and 2) percent UTD by time of NICU discharge/transfer. Timeliness of vaccination was also evaluated. Our balancing measure was the number of infants who had blood culture drawn within 48 hours following vaccine administration. T-tests and ANOVA were used for normally distributed data, and Kruskal-Wallis and Mann-Whitney tests for non-parametric data.
Results: Identified barriers to timely vaccination were concerns over infant stability, upcoming procedures requiring anesthesia, lack of urgency and staff being unaware of vaccine status and schedule. Prior to any interventions, vaccination rate at time of transfer/discharge was >65% UTD. During the intervention period, UTD vaccination rates peaked at 88%, with a nadir of 51% and a mean of 74% (Fig. 2). There was no disparity in vaccination rates based on Race/Ethnicity; Payer (private or public) and English versus Non-English speaking. There was no increase in blood culture rates during our study. Medical patients were more likely to be UTD than surgical patients on our weekly audits (Fig. 3).
Conclusion(s): Our quality improvement initiative led to a modest improvement in UTD vaccination status at time of NICU discharge/transfer. Ongoing studies include creating an education tool on vaccines safety and lack of contraindication, investigating the effect of parental perspectives, and utilizing the electronic medical record systems to alert providers of vaccine eligibility.
Figure 1: Key Driver Diagram
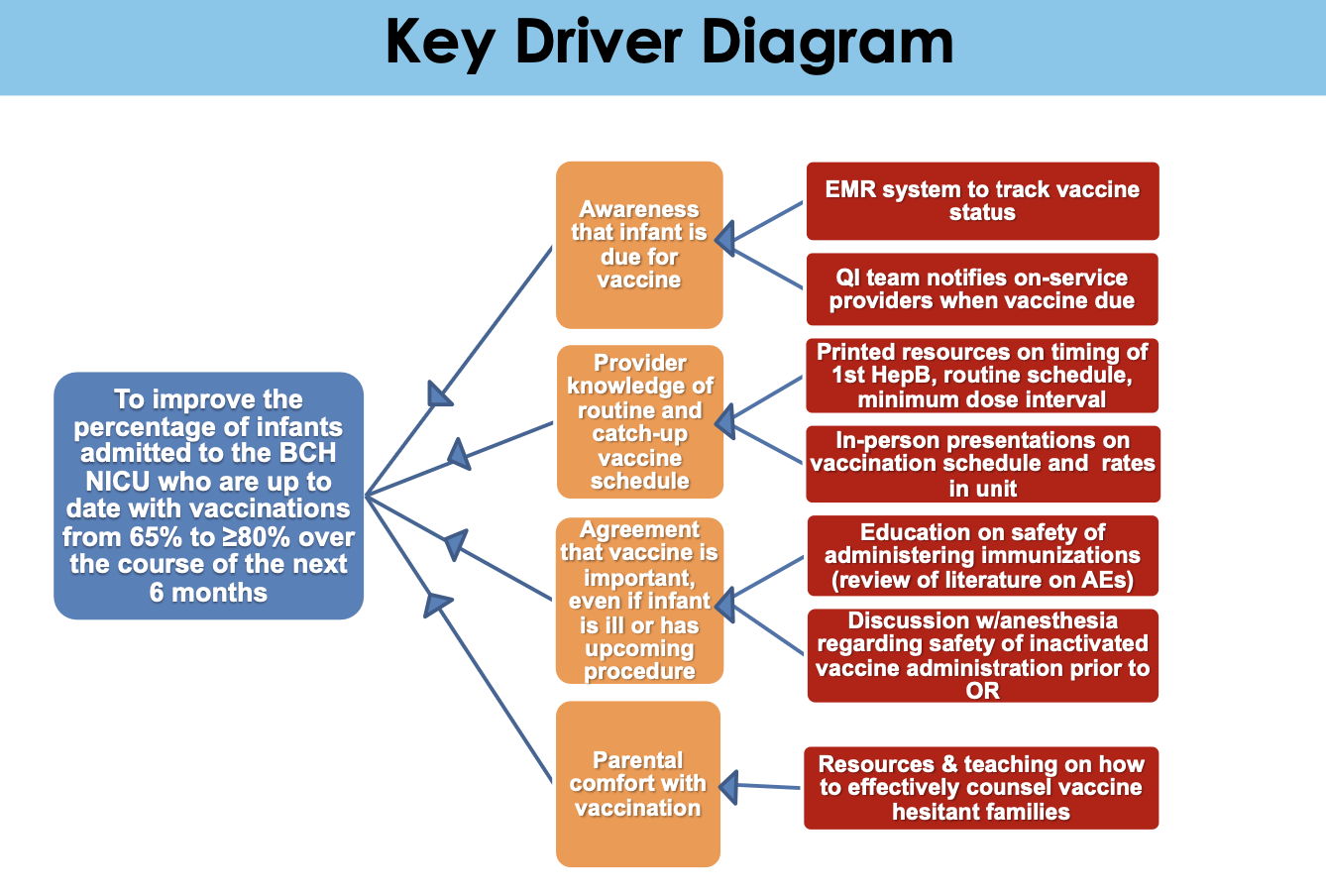 Abbreviations: AE-adverse events, BCH-Boston Children’s Hospital, EMR-electronic medical records, HepB- Hepatitis B vaccine, OR- operating room, QI-quality improvement.
Abbreviations: AE-adverse events, BCH-Boston Children’s Hospital, EMR-electronic medical records, HepB- Hepatitis B vaccine, OR- operating room, QI-quality improvement.Figure 2: Vaccine Timeliness Process Control Chart
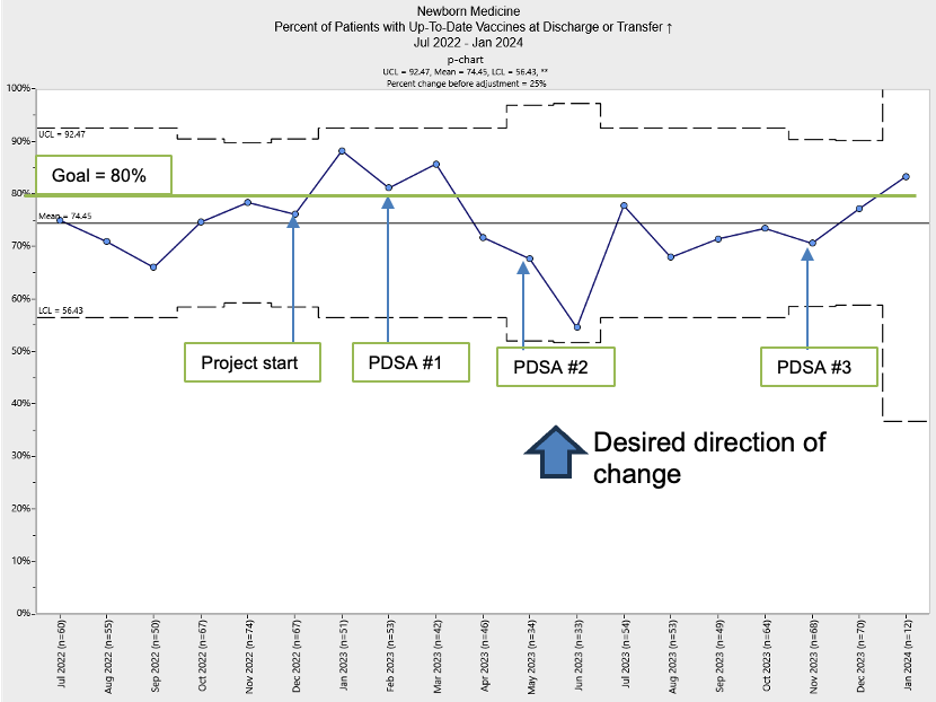 Percent of infants who were up-to-date (UTD) on vaccines at time of discharge/transfer from the Boston Children’s Hospital NICU during the study period (July 2022 to Jan 2024). PDSA cycles depicted in green, monthly rate in blue with goal line at 80% (in green). PDSA Phases: (1) reviewing vaccination status on medical rounds once a week, (2) increasing visibility and awareness with routine healthcare maintenance requirements by placing tracking stickers on the rounding folders, and (3) weekly pharmacy audit and email to increased awareness of vaccination rates prior to discharge within the NICU.
Percent of infants who were up-to-date (UTD) on vaccines at time of discharge/transfer from the Boston Children’s Hospital NICU during the study period (July 2022 to Jan 2024). PDSA cycles depicted in green, monthly rate in blue with goal line at 80% (in green). PDSA Phases: (1) reviewing vaccination status on medical rounds once a week, (2) increasing visibility and awareness with routine healthcare maintenance requirements by placing tracking stickers on the rounding folders, and (3) weekly pharmacy audit and email to increased awareness of vaccination rates prior to discharge within the NICU. Figure 3: Weekly Pharmacy Audit of Vaccination Status
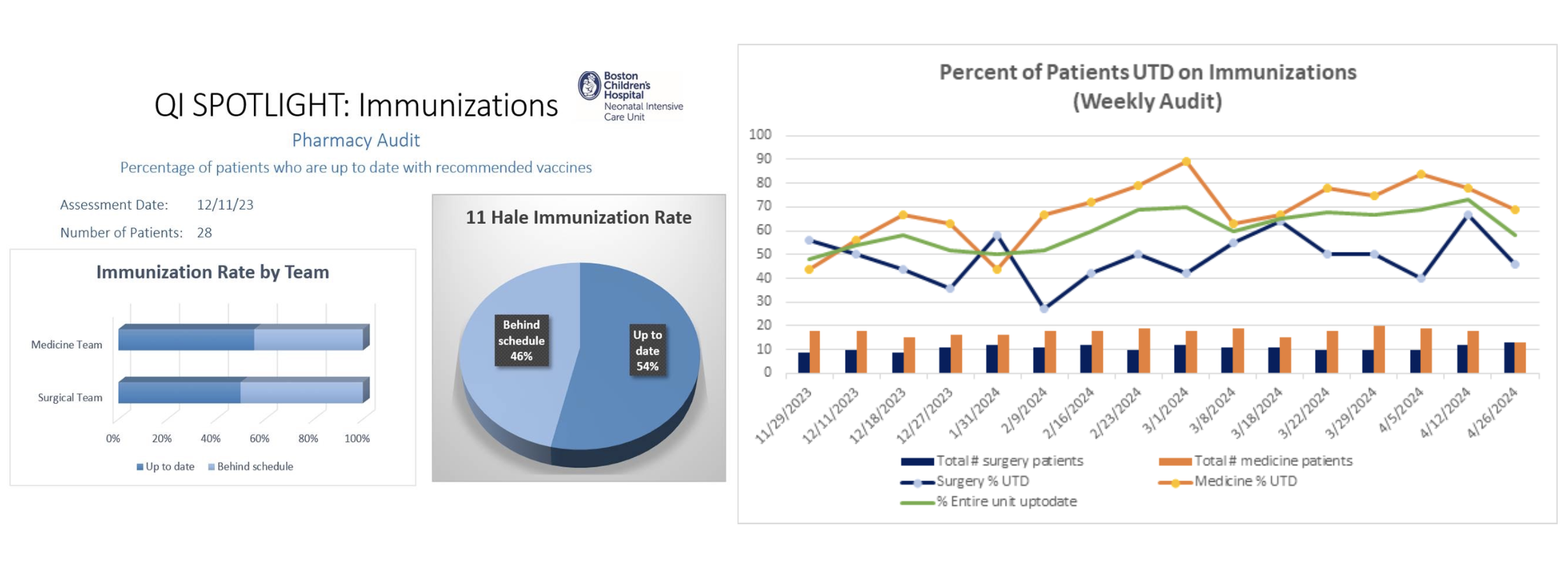 Sample QI spotlight email notification containing rates of up-to-date (UTD) vaccination of infants admitted to Boston Children’s Hospital NICU (left panel) and a longitudinal graph showing differences between the medical and surgical patients (right panel).
Sample QI spotlight email notification containing rates of up-to-date (UTD) vaccination of infants admitted to Boston Children’s Hospital NICU (left panel) and a longitudinal graph showing differences between the medical and surgical patients (right panel).

