Neonatal Hemodynamics and Cardiovascular Medicine 3
Session: Neonatal Hemodynamics and Cardiovascular Medicine 3
070 - Left ventricular dimensions at near term in extremely preterm infants: a prospective 4D-echocardiography study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 70.5773
Silvia Nogara, Università degli Studi di Verona, Vicenza, Veneto, Italy; Carolina Michel-Macías, UNAM, Queretaro, Queretaro de Arteaga, Mexico; Shiran S. Moore, Tel Aviv University, Port Washington, NY, United States; Audrey Hebert, CHU de Quebec - Universite Laval, Quebec city, PQ, Canada; Nina Nouraeyan, Jewish General Hospital, Verdun, PQ, Canada; Christine Drolet, Chu de Quebec/Laval University, Quebec, PQ, Canada; Anie Lapointe, CHU Ste-Justine, Montreal, PQ, Canada; Andréanne Villeneuve, CHU Sainte-Justine, Montréal, PQ, Canada; Brahim Bensouda, Université de Montreal, Montréal, PQ, Canada; Daniela Villegas Martinez, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Jessica Simoneau, Montreal Children’s hospital, Vercheres, PQ, Canada; Tiscar Cavalle-Garrido, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Adrian Dancea, MCH of MUHC, Montreal, PQ, Canada; Guilherme Sant'Anna, McGill University, Montreal, PQ, Canada; Gabriel Altit, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada
- SN
Silvia Nogara (she/her/hers)
Neonatologist
Università degli Studi di Verona
Vicenza, Veneto, Italy
Presenting Author(s)
Background: Studies in ex-preterm young adults revealed altered cardiac development, including smaller left ventricles. Prematurity outcomes and cardiovascular risks also showcase sex differences. Four-dimensional echocardiography (4D-ECHO) provides a more precise assessment of left ventricular (LV) volumes through LV segmentation. Importantly, early detection of postnatal cardiac changes and modifiers, such as sex, may guide risk profiling and targeted interventions in survivors from extreme prematurity.
Objective: Assess the impact of sex, gestational age (GA) and birth weight (BW) on LV end-diastolic volume (LV-EDV) obtained by 4D-ECHO.
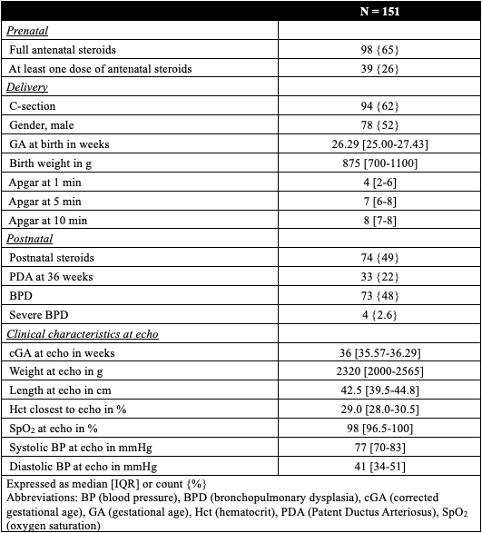
Design/Methods: Prospective, observational, single-center cohort study nested within the larger multicentric NORDIC-PREM study. Extremely preterm infants ( < 29 weeks) admitted to the neonatal unit of the Montreal Children’s Hospital between 2019 and 2023 were eligible. Newborns with significant congenital heart disease or genetic disorders were excluded. 4D-ECHO was performed at 35 to 37 weeks cGA using a Philips X7-2 probe. The relationships between LV-EDV and birth weight, as well as sex were analyzed using multiple regression. Models were adjusted for the presence of a patent ductus arteriosus (PDA) at 4D-ECHO and bronchopulmonary dysplasia (BPD). Images were analyzed offline by a blinded expert using TomTEC Arena.
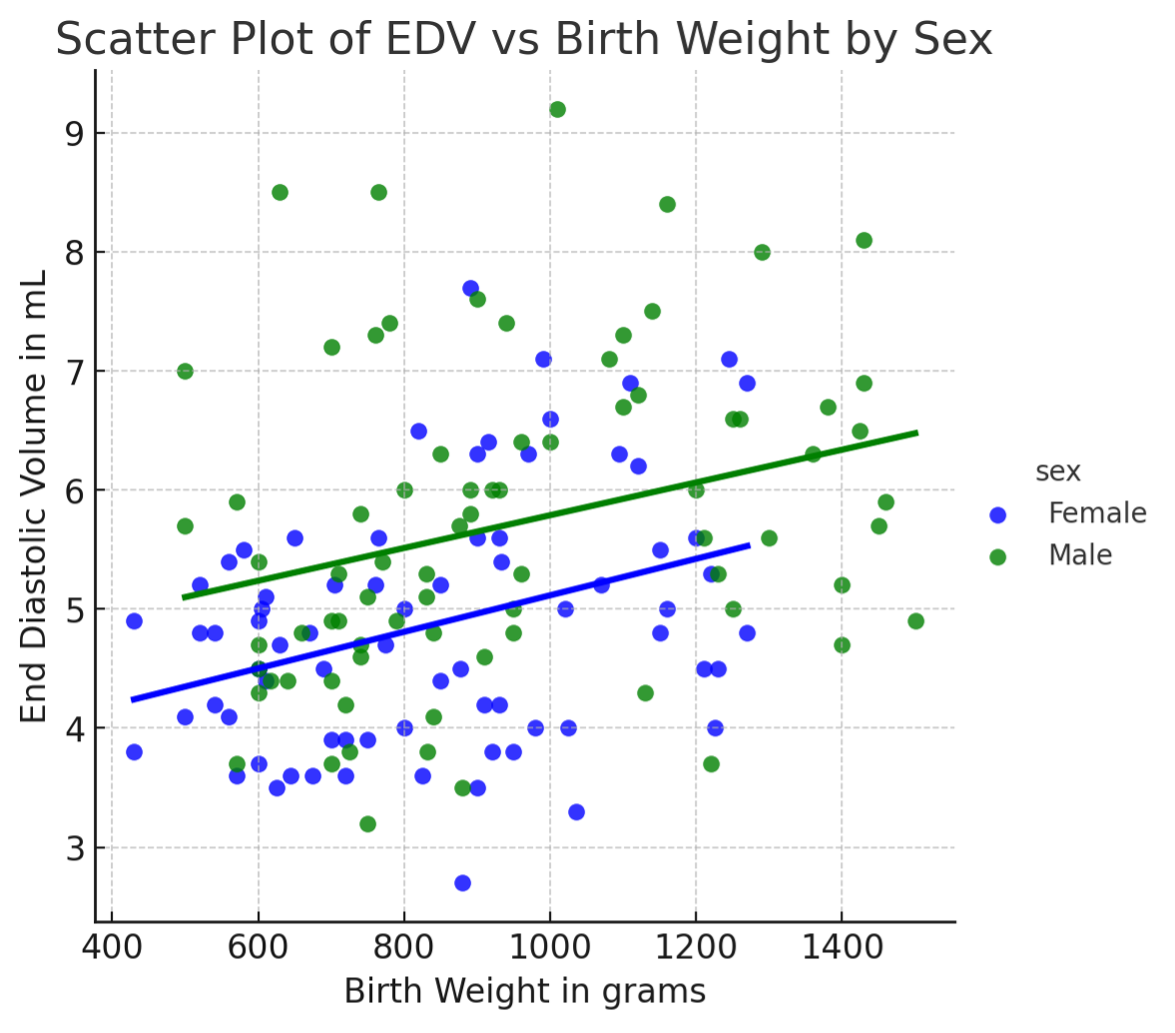
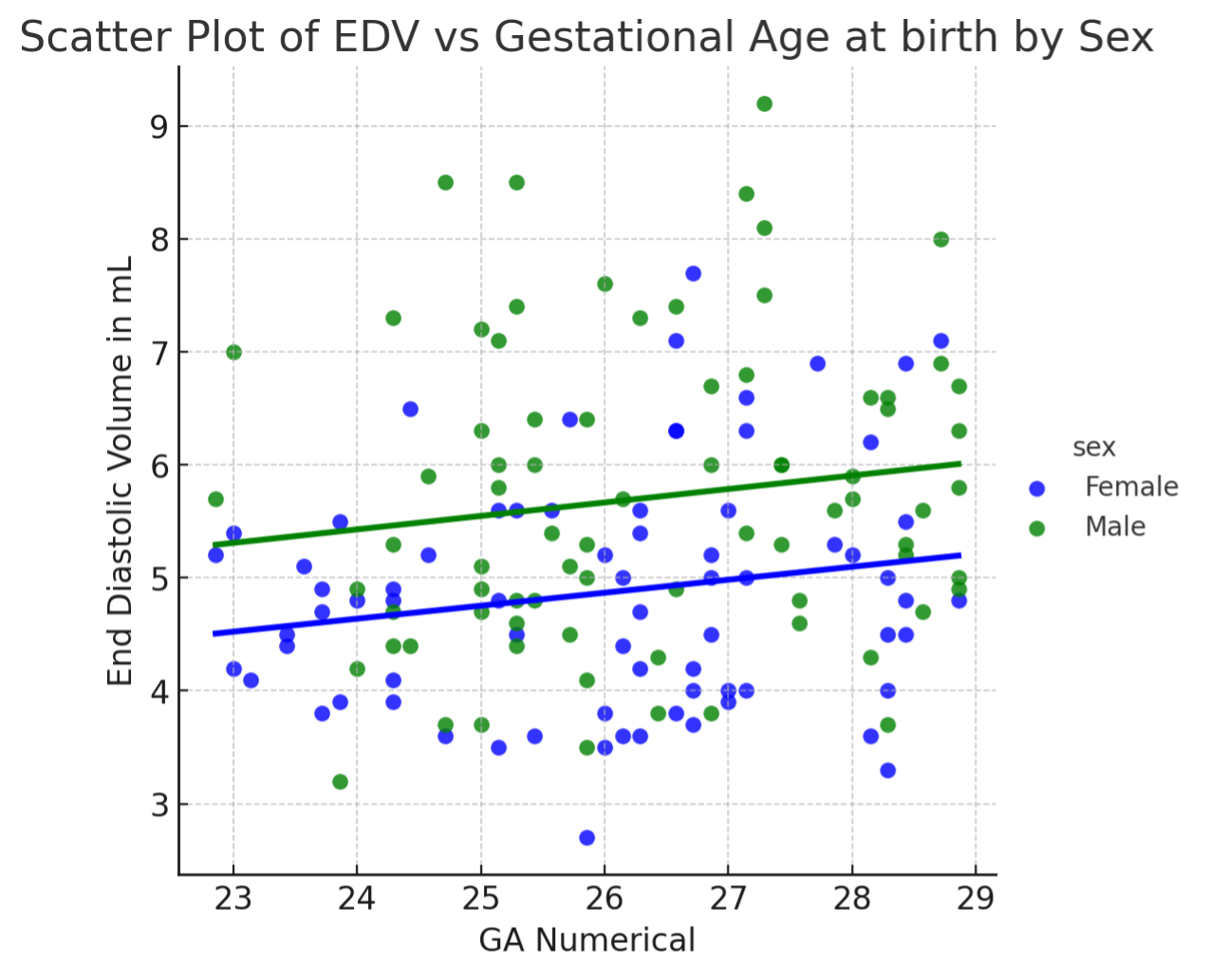
Results: Of 314 newborns assessed for eligibility, 171 were recruited, with 151 4D-ECHOs suitable for analysis. The cohort had a median GA of 26.3 weeks (IQR: 25.0–27.4) and a median birth weight of 875 grams (IQR: 700–1100) [Figure 1]. Graphically, LV-EDV was positively related to GA and birth weight, with significant sex-based differences [Figures 2 and 3]. LV-EDV was significantly associated with sex (β -0.54, 95% CI -0.92; -0.16, p< 0.05) and birth weight (β=0.001, 95% CI 0.001; 0.002, p< 0.05), adjusted for cGA at 4D-ECHO. After adjusting for PDA and BPD, these associations remained significant (sex: β=-0.54, 95% CI -0.92; -0.16, p< 0.05; birth weight: β=0.001, 95% CI 0.001; 0.002, p< 0.05). Further adjustment with exposure to steroids did not alter the strength of the association.
Conclusion(s): In our cohort, birth weight and sex are significantly associated with LV-EDV at 36 weeks cGA, as assessed by 4D-ECHO. Moreover, infants with lower GA and females had smaller LV-EDV by near-term corrected age, informing future research and personalized cardiac health assessments in this vulnerable population.
Demographic and clinical characteristics
LV-EDV vs Gestational Age by sex
LV-EDV vs Birth Weight by sex