Hospital Medicine 2: Quality Improvement
Session: Hospital Medicine 2: Quality Improvement
562 - Improving Critical Care Billing in a Hospital Medicine Division
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 562.5334
Bridget Allard, Children's National Health System, Washington, DC, United States; Dalton Haslam, Children's National Health System, Alexandria, VA, United States; Margarita Ramos, Children's National Hospital, Arlington, VA, United States; Padmaja Pavuluri, Children's National Health System, Washington, DC, United States; Paul Michel, Children's National Health System, Falls Church, VA, United States; Allison Markowsky, Children's National Health System, Stafford, VA, United States

Bridget Allard, DO (she/her/hers)
Attending Physician
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Professional billing provides the foundation for division revenue and is a vital component of delivering financially sustainable health care, yet provider knowledge is often lacking on how to optimally bill for varied clinical scenarios. Among our Hospital Medicine providers, baseline data showed that Critical Care Current Procedural Terminology (CPT) Evaluation and Management (E/M) codes were not being used despite provision of critical care services to our patients.
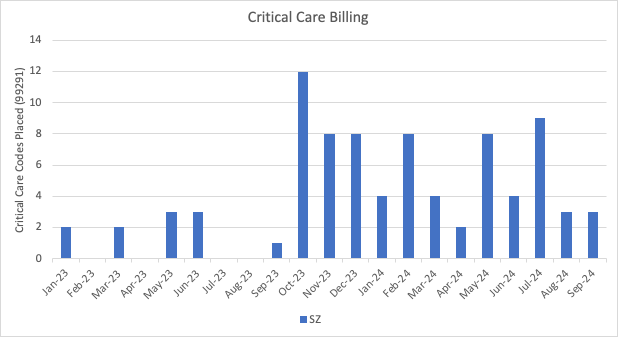
Objective: Our specific aim was to increase use of Critical Care CPT E/M codes by our division for patients on whom a rapid response was called and who met critical care criteria from 7% to 50% within 10 months and sustain for 6 months.
Design/Methods: This quality improvement effort was conducted from January 2023 through July 2024 in a 320 bed, free standing, academic, quaternary care children’s hospital. The Hospital Medicine division has an average daily census of 50 patients managed by residents, fellows and attendings. All daytime, weekday, hospital medicine rapid response team calls were included. Clinical scenarios that met the Centers for Medicare and Medicaid (CMS) critical care criteria were reviewed for placement of critical care charges. Key drivers for underutilization of Critical Care CPT E/M codes were identified and interventions developed which included educational sessions, a tip sheet, improved access to the billing codes in the electronic medical record (EMR), and regular data updates.
Results: Critical Care CPT E/M code usage increased from 7% to 50%. Retrospective chart review demonstrated appropriate clinical care 100% of the time the code was used and complete documentation to support use of the code was present 67% of the time. During the implementation phase 73 critical care charges were placed. This critical CPT E/M code carries a work relative value unit (wRVU) of 4.5 which per the current 2024 CMS Medicare wRVU rate of $32.24 would equal an additional minimum $145.08 per charge and an additional $10,590.84 cumulative of the 73 charges placed thus far in the project.
Conclusion(s): Educational interventions, just-in-time resources, and regular feedback on professional billing improve appropriate critical care billing code utilization and optimizes revenue to better reflect the variety and complexity of care provided. Next steps include optimizing provider documentation to support the use of appropriate codes and expanding to other sites within our regional network.
Percent of critical care RRT calls with an associated critical care charge placed
Critical Care p-chart.pdf
Absolute number of critical care charges placed