Hospital Medicine 1: Quality Improvement
Session: Hospital Medicine 1: Quality Improvement
551 - Improving Code Status Orders through Provider Awareness and Education for Children with Medical Complexities
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 551.5333
Jasmine Parker, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; James Bowen, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Rachel Peterson, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Laura Brower, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States
- JP
Jasmine Parker, Bachelors of Science
Clinical Research Professional
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Inaccurate code status orders (CSO) may result in children with medical complexity (CMC) receiving interventions incongruent with family wishes during emergent situations. CMC are at risk of high morbidity and mortality. Despite this, code status orders (CSO) were rarely placed during CMC admissions.
Objective: Using quality improvement methods, we sought to increase timely placement of CSOs for CMC admitted to the inpatient complex care hospital medicine service within 72 hours from approximately 5 % to 80% within six months.
Design/Methods: Our team designed a process map and used key drivers (Figure 1) to develop multiple Plan-Do-Study-Act cycles to improve timely CSO placement for CMC admitted to the hospital. Interventions targeted provider education on CSO, created a shared understanding of the importance of having code status discussions, and increased opportunities for providers to have these discussions. Our process measure, evaluated on a P-chart, was the percentage of CMC (grouped by five patients) who received a CSO within 72 hours of admission. Established rules were used to differentiate between common and special cause variation. The outcome measure was placement of an active CSO at the time of clinical deterioration (i.e. medical response team activation). The balancing measure was the rate of palliative care consultations. Outcome and balancing measures were evaluated pre-and post-intervention via chi-squared tests. Stakeholders (families, clinicians) were routinely engaged to obtain short term focused feedback on our interventions.
Results: Our interventions led to timely CSOs increasing from an average of 5% to 62% over eight months. The first shift to 40% came after disseminating education on performing code status. A second shift occurred after integrating CSO discussions into daily pre-rounds huddles. Patients with an active CSO at the time of clinical deterioration increased from 9% to 44% (p=0.04). Palliative care consultation rates remained relatively stable, increasing from 1% to 5% (p=0.16), post interventions. Feedback on our interventions were positive; clinicians noted hesitance in performing code status discussions via phone, which was the primary driver of “missed” CSO.
Conclusion(s): Integrating provider education and improving shared understanding of code status order placement led to increased code status discussions for families of CMC. Future interventions will target families unable to be at bedside. Future work will include the spread of these interventions to other clinical environments such as the intensive care unit.
Figure 1. Key Driver Diagram illustrating the intervention implemented during February 2024 through September 2024
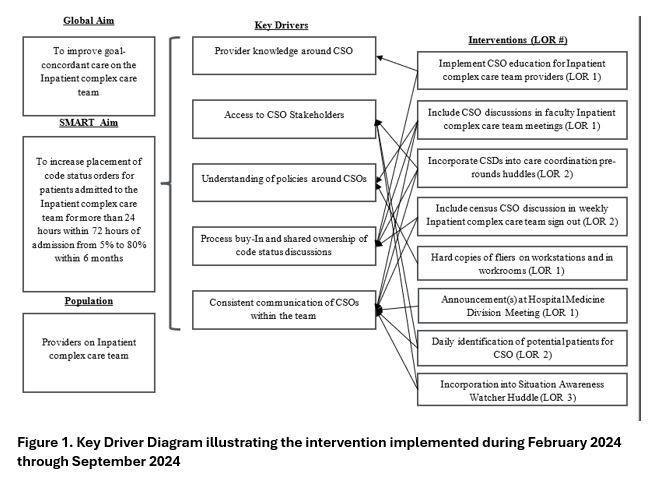
Figure 2. P-chart revealing the percentage of patients admitted to the Inpatient complex care team (CCT) for over 24 hours for which a timely code status order was placed. Data points include patients cohorted by five.
.jpg)


