Mental Health 1
Session: Mental Health 1
758 - Implementing a Comprehensive, Tiered, Mental Health Pathway within a Pediatric School-Based Health Clinic to Enhance Behavioral Health Integration and Improve Access to Mental Health Care for Students
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 758.5298
Karen C. Manotas, University of Utah Health, Salt Lake City, UT, United States; Kimberly Hansen, University of Utah School of Medicine, Salt Lake City, UT, United States; Carole H. Stipelman, University of Utah School of Medicine, Salt Lake City, UT, United States; justin Alvey, University of Utah School of Medicine, Salt Lake City, UT, United States; Tristan Peterson, University of Utah School of Medicine, Salt Lake City, UT, United States; Spencer Lee, University of Utah School of Medicine, Salt Lake City, UT, United States; jeff Robison, University of Utah School of Medicine, Salt Lake City, UT, United States

Karen C. Manotas, MD (she/her/hers)
Assistant Professor, Department of Psychiatry, Department of Pediatrics
University of Utah Health
Salt Lake City, Utah, United States
Presenting Author(s)
Background: In Utah, there are approximately 6 child psychiatrists for every 100,000 children in need of mental health services and 58% of children with a mental health diagnosis did not receive treatment in 2021. The average wait time for treatment is 2 months for psychotherapy and 6 months for adolescent psychiatry. School-based health centers (SBHC) have demonstrated effectiveness in improving access to healthcare. Comprehensive, tiered, mental health services co-located within a high school based primary care clinic may improve access and reduce wait times for behavioral health treatment.
Objective: Describe an innovative system that addresses equitable access, stratification, and triage of mental health care needs within a SBHC as a means to effectively and efficiently and provide timely access to adolescent behavioral health services in a time of a mental health crisis.
Design/Methods: A multi-tiered, full service behavioral health triage system was implemented with a referral system from the primary care clinic that included universal mental health screening (Figure 1.). Wait times from referral to behavioral health appointment were calculated and compared to Utah state data. Averages were reported as mean ± SD and compared with t-test. Demographics, body weight index (BMI), service utilization, and mental health screening were compared in visits with and without a mental health diagnosis using χ2-test (Table 1.).
Results: More than a third of the high school clinic visits included a mental health diagnosis. Visits for females, those covered by Medicaid, or a BMI ≥ 95th percentile were more likely to include a mental health diagnosis. With Hispanic/Latin X as the reference, visits with White and Native Hawaiian and Pacific Islander students were less likely to include a mental health diagnosis. Of 65 internal referrals to behavioral health, 36 had mean lag time calculated (all 36 patients; 4 ± 4.1 d) which was similar for patients receiving individual therapy (27 patients; 3.6 ± 4.1 d) vs psychiatry (9 patients; 5.2 ± 4.9 d; P = .3).
Conclusion(s): A multi-tiered, full service behavioral health system within a SBHC was associated with markedly decreased wait times.
Table 1. SBHC Demographics and Utilization
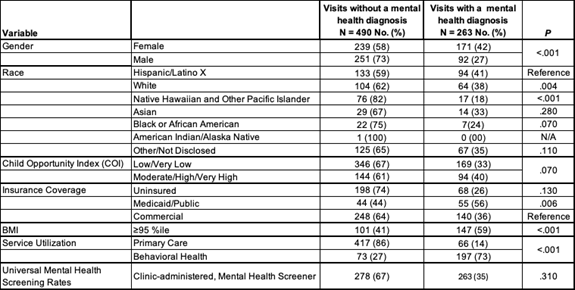 Table 1 Legend. Mental Health Screeners included Pediatric Symptom Checklist- Youth (35 item), Patient Health Questionnaire for Adolescents, and Generalized Anxiety Disorder 7-item.
Table 1 Legend. Mental Health Screeners included Pediatric Symptom Checklist- Youth (35 item), Patient Health Questionnaire for Adolescents, and Generalized Anxiety Disorder 7-item.Figure 1. Tiered, SBHC Mental Health Referral Pathway with Behavioral Health Integration
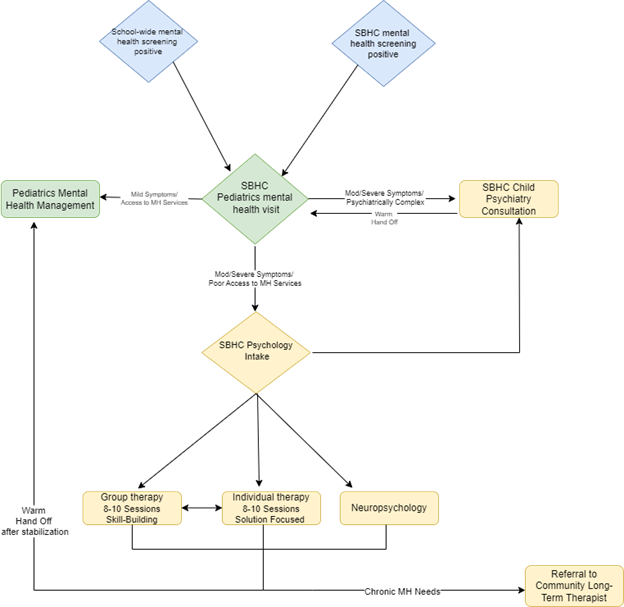 Figure 1 Legend. Blue Diamonds: Tier 1 universal mental health screening as clinic referral sources to School-Based Health Center pediatricians for mental health screening visit.
Figure 1 Legend. Blue Diamonds: Tier 1 universal mental health screening as clinic referral sources to School-Based Health Center pediatricians for mental health screening visit.Green Diamond: Tier 2 Pediatrics Screening Visit for medical clearance and decision making and primary triage of mental health needs.
Yellow Diamond: Tier 3 Internal Behavioral Health consultation and further stratification of mental health needs based on Intake Assessment and/or Psychiatry evaluation. Upon stabilization of presenting problem and/or attainment of treatment plan goal, warm hand off back to pediatrician. If a patient requires specialized long term therapy, the patient is routed to the clinic coordinator for assistance with community therapy referral.

