Neonatal Nephrology/AKI 2
Session: Neonatal Nephrology/AKI 2
024 - Investigating Associations between Neonatal Acute Kidney Injury and Parental Assessment of Neurodevelopment
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 24.5305
Jeffrey E. King, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Olivia Kinsinger, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Molly Mead, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Megan Rodgers, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Amy L. Ruddy-Humphries, MUSC, CHARLESTON, SC, United States; Cassandra Coleman, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; David Selewski, Medical University of South Carolina, Mount Pleasant, SC, United States; Jill C.. Newman, Medical University of South Carolina College of Medicine, Mount Pleasant, SC, United States; Heidi J.. Steflik, Medical University of South Carolina College of Medicine, Charleston, SC, United States

Jeffrey E. King, MD (he/him/his)
Fellow Physician
Medical University of South Carolina College of Medicine
Charleston, South Carolina, United States
Presenting Author(s)
Background: Associations between neonatal acute kidney injury (AKI) and early childhood neurodevelopmental outcomes remain understudied.
Objective: Investigate associations between neonatal AKI in very low birthweight (VLBW, < 1,500 grams) infants and subsequent parental assessment of neurodevelopment. Hypothesis: AKI is associated with neurodevelopmental impairment (NDI) recognized by parental questionnaire in early childhood.
Design/Methods: Single-center, retrospective cohort study of VLBW infants cared for at the Medical University of South Carolina (MUSC) neonatal intensive care unit (NICU) between 2018-2020 and subsequently evaluated in the MUSC NICU Developmental Clinic between 18 and 35 months of age with completion of parental questionnaires assessing development. Neonatal AKI was diagnosed using the modified, neonatal Kidney Disease: Improving Global Outcomes (KDIGO) serum creatinine criteria.
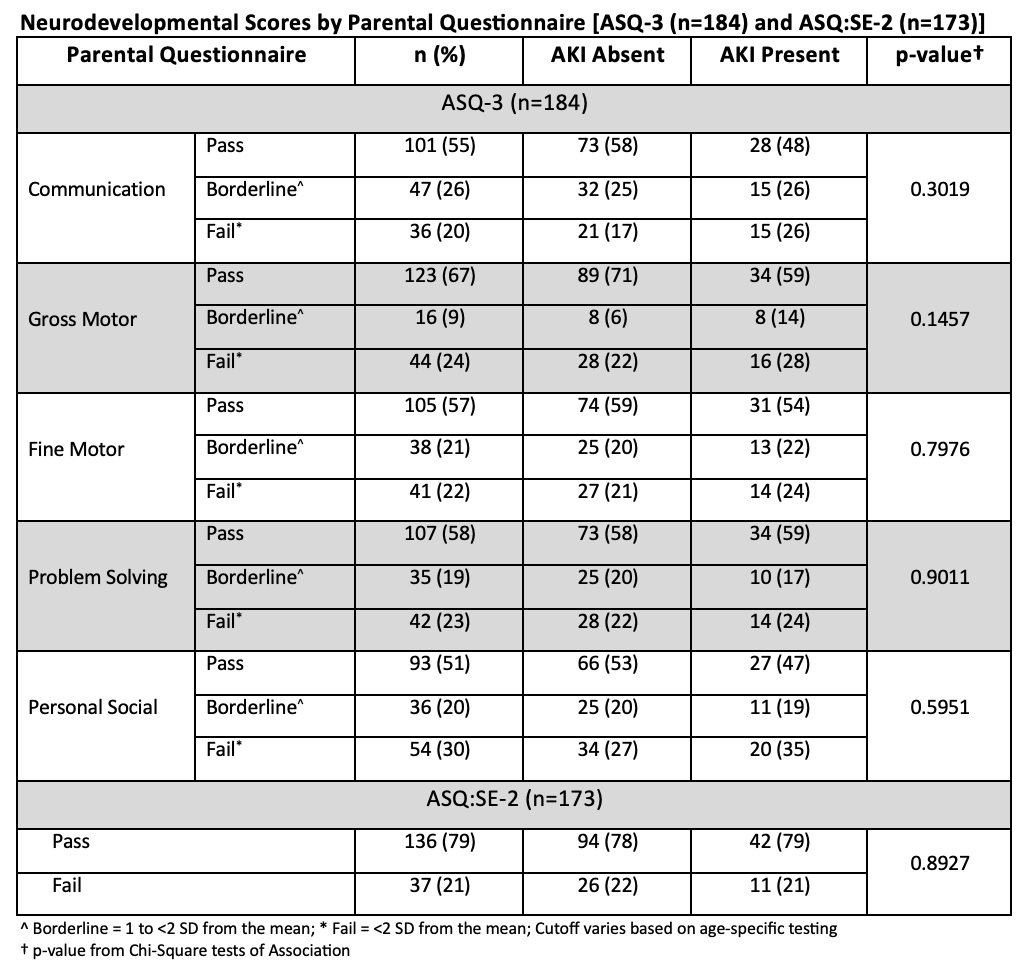
The primary outcome, parental assessment of neurodevelopment, was determined using the Ages & Stages Questionnaires, Third Edition (ASQ®-3) and the Social-Emotional questionnaire component (ASQ®-SE-2). The ASQ®-3 assesses five developmental domains (Communication, Gross Motor, Fine Motor, Problem Solving, and Personal-Social). For each ASQ®-3 domain and ASQ®-SE-2, reported scores are compared to established age-specific developmental cutoffs and given a designation of Pass, Borderline, or Fail (only Pass or Fail for ASQ®-SE-2). Borderline scores fall within a validated range near the cutoff value while Pass and Fail scores are above and below this value, respectively. NDI was defined by the presence of ‘Fail’ scores in any ASQ®-3 domain or on the ASQ®-SE-2.
Results: Of 203 infants included, 64 (32%) experienced neonatal AKI. Neonates with AKI had lower birthweight (AKI: 829 ± 211 grams vs no AKI: 1,110 ± 259 grams) and younger gestational age (26.0 ± 2.1 weeks’ vs 28.8 ± 2.3 weeks’) with longer lengths of hospitalization (110 [89,128] days vs 65 [40,90] days) (all p< 0.02).
In total, 184 (91%) infants had completed ASQ®-3 and 173 (85%) had completed ASQ®-SE-2 by their caregivers. The majority (>50%) of all neonates passed each ASQ® domain. When comparing results between those with and without AKI, no statistically significant differences were detected in any ASQ®-3 domain or ASQ®-SE-2 (Figure).
Conclusion(s): In this cohort, neonatal AKI is not associated with NDI as assessed with parental development questionnaire, though further investigations with larger sample sizes are warranted.
Neurodevelopmental Scores by Parental Questionnaire (Bar Graph)
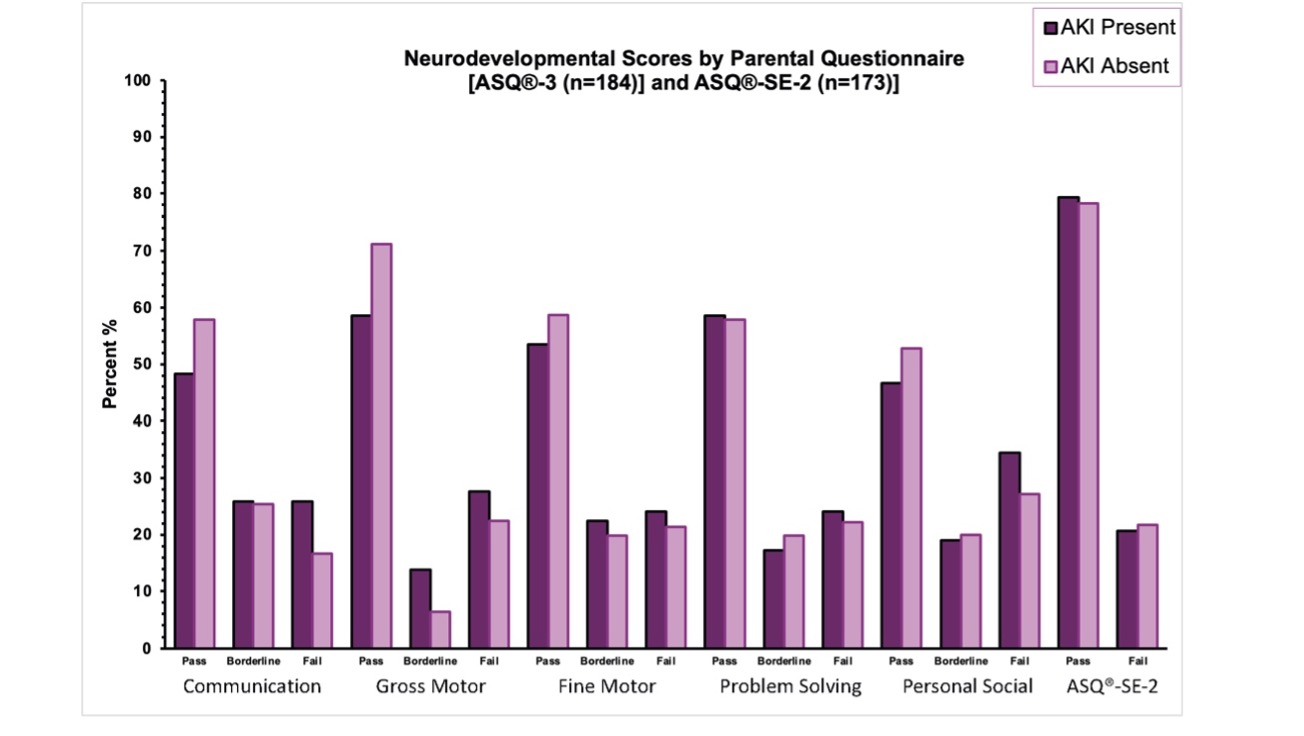
Neurodevelopmental Scores by Parental Questionnaire (Table)