Hospital Medicine 2: Quality Improvement
Session: Hospital Medicine 2: Quality Improvement
566 - Medication Overdose Admission Algorithm in a Tertiary Children’s Hospital
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 566.5586
Jody Huber, Sanford Children's Hospital, Sioux Falls, SD, United States; Patrizia Scali, University of South Dakota, Sanford School of Medicine, Sioux Falls, SD, United States; Rachel Koshiol, University of South Dakota, Sanford School of Medicine, Rapid City, SD, United States; Alexandra L. Kracht, University of South Dakota, Sanford School of Medicine, Sioux Falls, SD, United States; Emily Petersen, University of South Dakota, Sanford School of Medicine, Sioux Falls, SD, United States; Anthony Restaino, University of South Dakota, Sanford School of Medicine, Sioux Falls, SD, United States; John S. Vassar, University of South Dakota, Sanford School of Medicine, Rapid City, SD, United States; Gokhan Olgun, Sanford Children's Hospital, Sioux Falls, SD, United States

Patrizia Scali, MD
Pediatrics Resident
University of South Dakota, Sanford School of Medicine
Sioux Falls, South Dakota, United States
Presenting Author(s)
Background: Deliberate pharmacologic ingestion with the intent of self-harm is a critical diagnosis in the pediatric population which requires appropriate triaging. Admission to the general pediatric floor versus pediatric intensive care unit (PICU) is pivotal for optimal outcomes, patient safety and resource utilization.
Objective: This study is a quality improvement project that assesses the impact and safety of newly implemented admission criteria developed through multidisciplinary collaboration in a tertiary care center.
Design/Methods: This was a pre- and post-intervention study of 155 patients 10 to 18 years of age with a diagnosis of pharmacologic ingestion or overdose with intent for self-harm admitted to a pediatric tertiary care center between January 1, 2020, and December 31, 2022. Patients were divided into pre-intervention and post-intervention groups. The intervention was the development and implementation of an admission criteria protocol created in collaboration with pediatric hospitalists, intensivists, cardiologists, emergency medicine physicians, inpatient nursing leadership, and a toxicologist.
Patient data was collected from the electronic medical record and included demographic characteristics, clinical parameters, and outcomes. A statistical analysis was performed on the data using the software R.
Continuous data was presented as values, standard deviations, and percentages. Chi-square was used to analyze changes in admission patterns and unwanted transfers, while an unpaired t-test assessed differences in the total duration of hospitalization. A p-value of less than 0.05 was considered statistically significant.
Results: Baseline demographics were comparable between groups, with no significant difference in age, sex, race, or insurance status (Table 1). The study showed a significant reduction in admissions to the PICU post-intervention, with no increase in adverse outcomes such as escalation to the PICU or death (Table 2). No transfers from the general pediatric floor to the PICU were observed in either group. Protocol compliance in the post-intervention group was 85%, indicating adherence.
Conclusion(s): Well-defined admission criteria for pediatric patients with intentional ingestion significantly improved admission practices and safeguarded PICU resources without increased transfers to PICU or mortality, indicating patient safety. These results demonstrate the importance of implementing standardized protocols to enhance pediatric patient care.
Table 1. Demographics
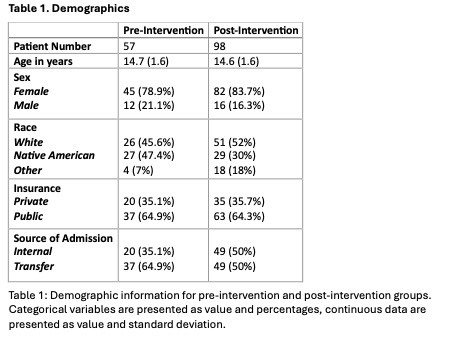 Table 1: Demographic information for pre-intervention and post-intervention groups. Categorical variables are presented as value and percentages, continuous data are presented as value and standard deviation.
Table 1: Demographic information for pre-intervention and post-intervention groups. Categorical variables are presented as value and percentages, continuous data are presented as value and standard deviation.Table 2. Outcomes
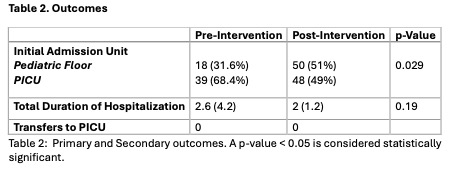 Table 2: Primary and Secondary outcomes. A p-value < 0.05 is considered statistically significant.
Table 2: Primary and Secondary outcomes. A p-value < 0.05 is considered statistically significant. Table 1. Demographics
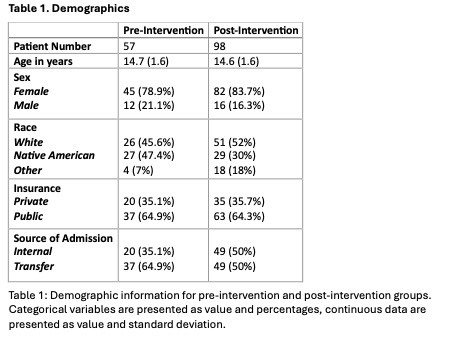 Table 1: Demographic information for pre-intervention and post-intervention groups. Categorical variables are presented as value and percentages, continuous data are presented as value and standard deviation.
Table 1: Demographic information for pre-intervention and post-intervention groups. Categorical variables are presented as value and percentages, continuous data are presented as value and standard deviation.Table 2. Outcomes
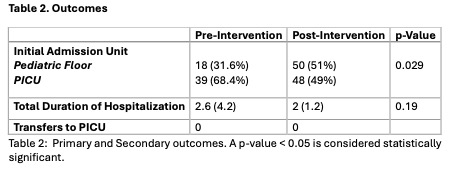 Table 2: Primary and Secondary outcomes. A p-value < 0.05 is considered statistically significant.
Table 2: Primary and Secondary outcomes. A p-value < 0.05 is considered statistically significant. 
