Mental Health 2
Session: Mental Health 2
776 - Meeting the Need: A Mental Health Toolkit for Disaster Response Efforts
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 776.5585
Patty A. Davis, Children's Mercy Kansas City, Lake Lotawana, MO, United States; Kristin L. Ray, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Angela Guzman, Children's Mercy, Kansas City, MO, United States; Morgin Dunleavy, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States

Patty A. Davis, LSCSW, LCSW, IMH-E-III (she/her/hers)
Program Manager, Trauma Informed Care
Children's Mercy Kansas City
Lake Lotawana, Missouri, United States
Presenting Author(s)
Background: Inhale courage, exhale fear. An overwhelming feeling that swept through our community following a senseless act of violence. Following a mass shooting event our pediatric hospital quickly identified mental health (MH) as a priority in our disaster response. Addressing the psychological impact on children, families, community members, and staff was a critical focus for an organization-wide strategic response. We rapidly mobilized trauma response efforts to cover those most impacted and shore up access to MH resources and education to meet the demand following this event.
Objective: Develop a response plan that includes education and resources on managing appropriate dialogue with children about traumatic events, recommendations to mitigate fears and uncertainties, and advisement on when to seek professional MH support. Model MH triage and increase access to trauma-focused MH interventions. Ensure hospital team members receive immediate MH support offerings resulting from secondary trauma and other barriers to wellbeing following a disaster.
Design/Methods: We used a qualitative, descriptive approach by connecting with MH disaster response specialists internally and across the country to identify trending and evidence-informed response strategies. Hospital and community stakeholder meetings provided a venue to share resources and maintain open dialogue to increase caregiver confidence in addressing trauma and mitigate gaps in our MH referral systems. For staff MH support, we elevated on-site counseling services, team reflections, and established respite space. Long-term interventions included free training for community caregivers on disaster response skills, trauma-focused MH interventions, and development of a trauma referral navigator.
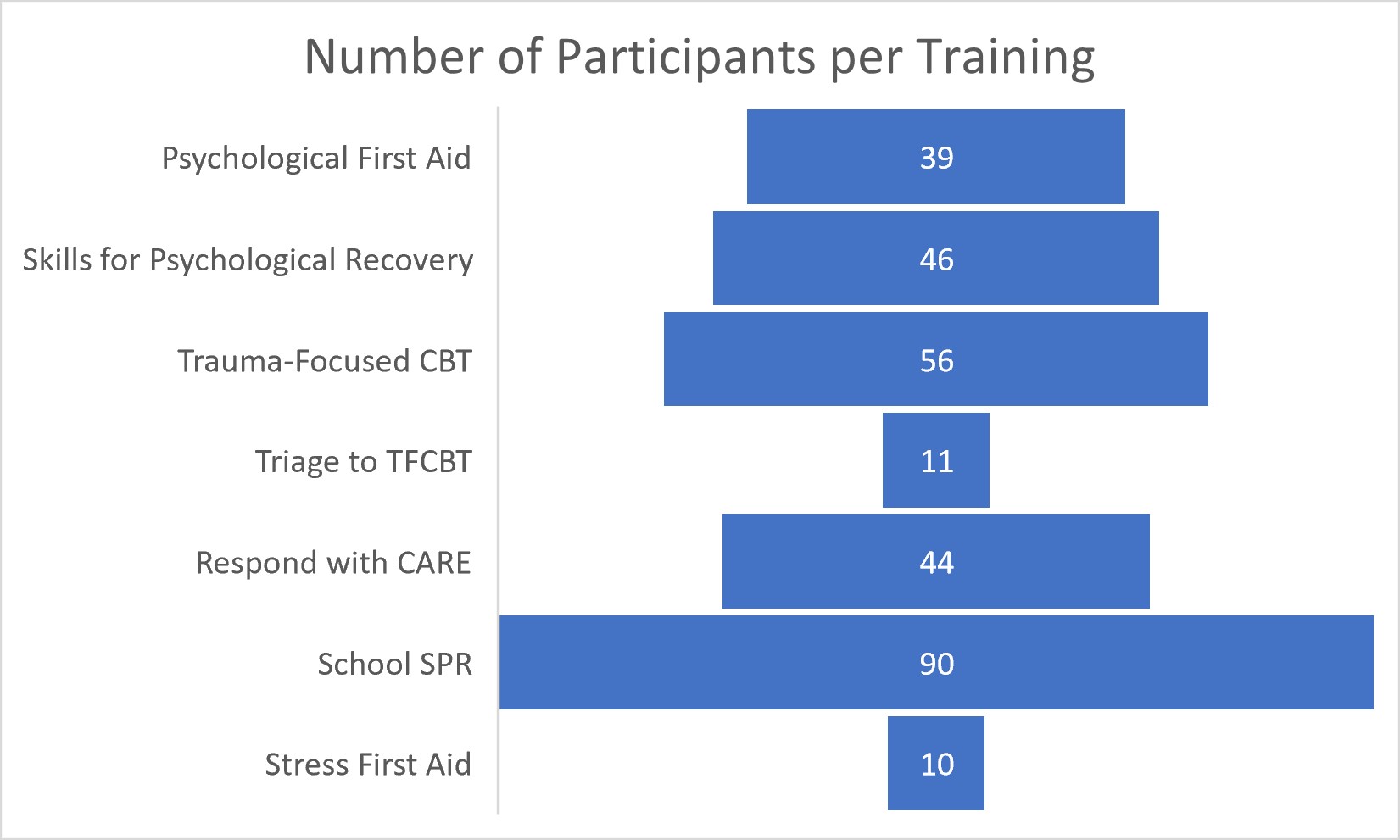
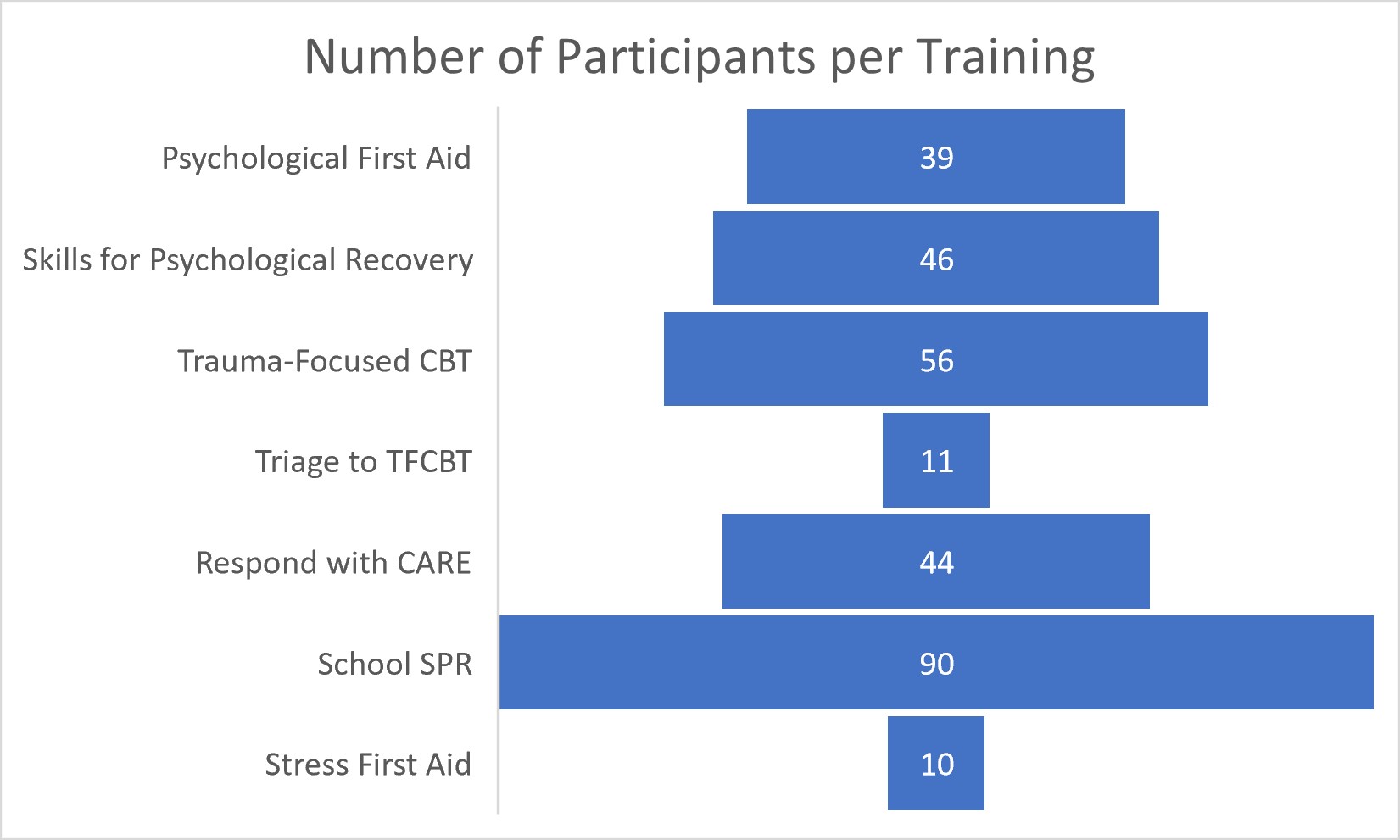
Results: We reached 87 community partners. Out of the 403 community caregivers who shared interest in learning more about behavioral health disaster response, 282 people from 77 different organizations attended at least one of the trainings within 6 months. In addition to community impact, the hospital was able to reach 1600 employees through a variety of MH offerings.
Conclusion(s): It is no longer a matter of if, it’s when. MH support following disasters cannot be an afterthought. Our healthcare team collaborated across the enterprise and with community partners to develop and disseminate a highly strategic disaster response including MH support as a top priority for the patients, families, community, and staff members alike. As we move forward, we have a framework for future disaster responses to address the ongoing MH needs of the workforce and the community we serve.
Number of Participants Per Disaster Response Training
Number of Different Community Partners per Field at Trainings and Stakeholder Meetings
.png)
Post-Disaster Staff Support Interventions
.jpg)
Number of Participants Per Disaster Response Training
Number of Different Community Partners per Field at Trainings and Stakeholder Meetings
.png)
Post-Disaster Staff Support Interventions
.jpg)

