Emergency Medicine 5
Session: Emergency Medicine 5
266 - Naloxone Distribution in the Pediatric Emergency Department: A Pilot Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 266.5614
Jake R. Lehman, Children's Hospital Los Angeles, Los Angeles, CA, United States; Gabriel Devlin, Children's Hospital Los Angeles, Los Angeles, CA, United States; Ameer P. Mody, Children's Hospital Los Angeles, Los Angeles, CA, United States

Jake R. Lehman, MD (he/him/his)
Pediatric Resident
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Community naloxone distribution is a key pillar in the public health response to the opioid epidemic. Although emergency departments (EDs) are critical access points for many children, the feasibility of pediatric ED-based naloxone distribution is untested.
Objective: To demonstrate the feasibility of a naloxone distribution program for at-risk patients presenting to a pediatric ED.
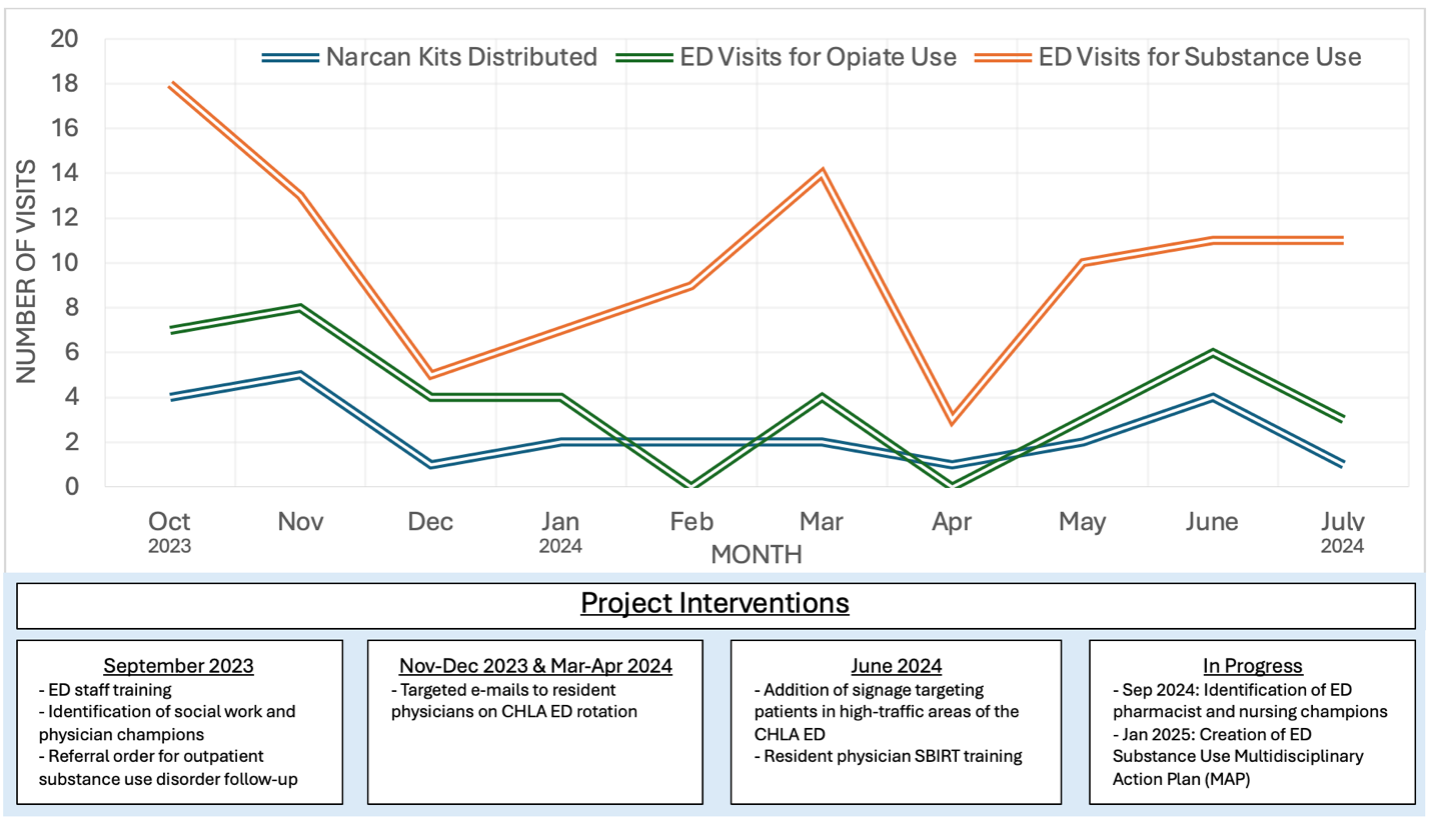
Design/Methods: We obtained intranasal naloxone through the California Naloxone Distribution Project, which we used to develop an 'opioid overdose kit’ (Figure 1). Kits were stored in the ED and could be given by any ED staff member who completed a 15-minute training workshop. The target population was ED patients presenting with substance use or mental health concerns, but kits could be given to any patient or family member. Kit recipients were educated on recognizing opioid overdose and how to use naloxone. Additional interventions were later implemented to increase distribution (Figure 2). Naloxone distribution began on September 27, 2023. After a 10-month pilot period, we performed a retrospective chart review of all ED encounters with an ICD-10 diagnosis of substance use or overdose. We then measured monthly kit distribution, as well as patient- and provider-level descriptive statistics.
Results: We trained 44 attending physicians, 124 physician trainees, 53 nurses, and 8 social workers on ED naloxone kit distribution. We distributed 24 naloxone kits to 20 patients between 12 and 22 years old (average 16.4 years) over the study period. Kits were dispensed to patients with an acute substance use concern (79%), opioid prescription without concern for substance use disorder (13%), and provider concern for substance use disorder despite an unrelated chief concern (8%). Among patients who were discharged with naloxone, none had suicidal ideation. Physicians issued most kits (70%), followed by social workers (30%). 100% of patients who received the kit also received opioid overdose and nasal naloxone training. 21% (range 7-38% per month) and 44% (range 25-100% per month) of ED encounters for any substance use and for opiate use, respectively, received naloxone.
Conclusion(s): Pediatric ED naloxone distribution is feasible. Future areas for quality improvement include (1) improving engagement among non-physician ED staff, (2) increasing distribution to patients with non-substance use visits (including systematic screening for substance use among patients), and (3) electronic medical record-based best practice advisories based on discharge diagnoses.
Figure 1. Example of an ‘opioid overdose kit’.
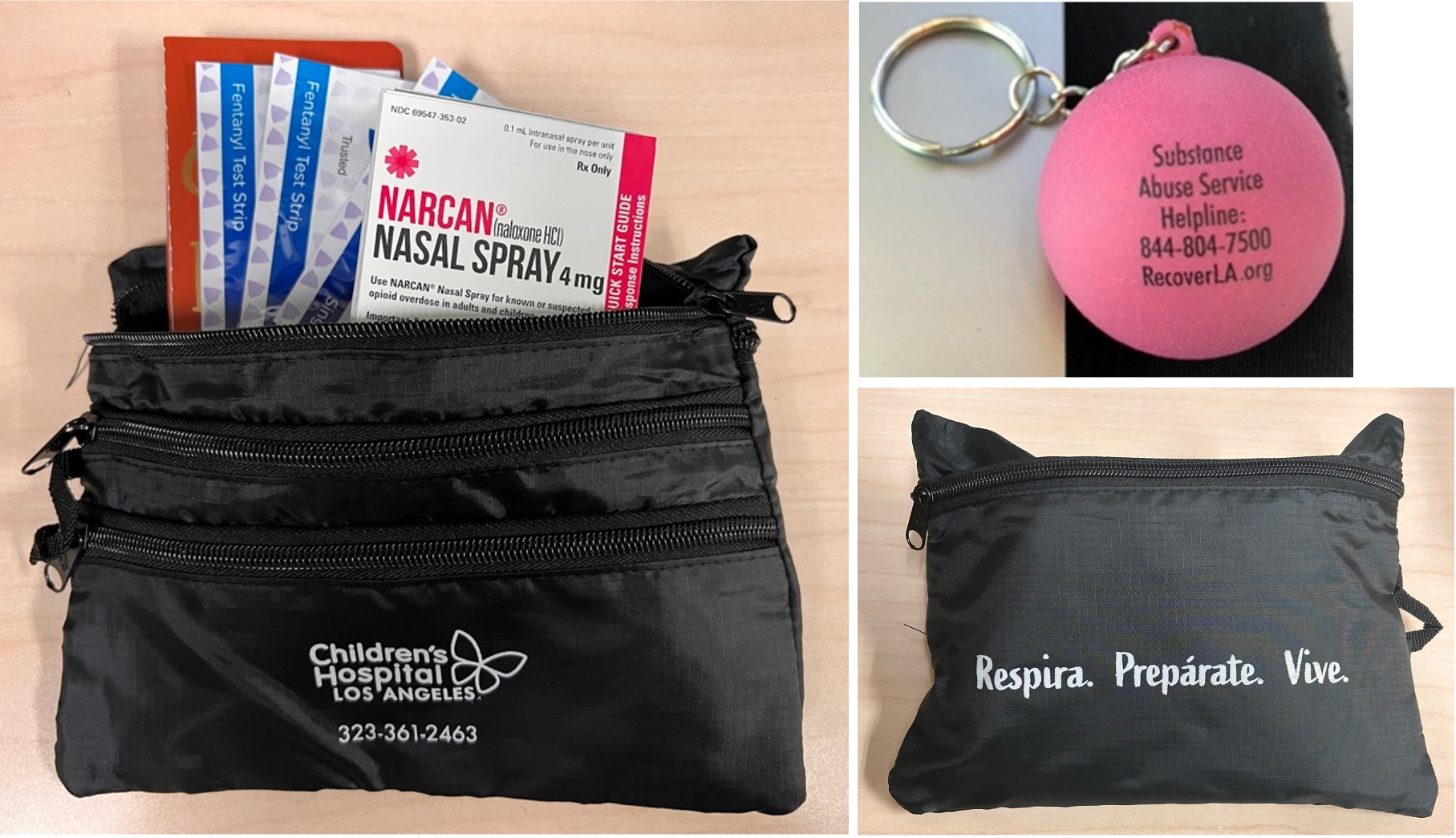 Naloxone kits included naloxone, fentanyl test strips, educational materials, and resources for outpatient substance use treatment. Kits were created in English, Spanish, Arabic, Armenian, Chinese, and Korean.
Naloxone kits included naloxone, fentanyl test strips, educational materials, and resources for outpatient substance use treatment. Kits were created in English, Spanish, Arabic, Armenian, Chinese, and Korean.Figure 2. Naloxone kit distribution compared to opiate and substance use monthly ED visits over time.
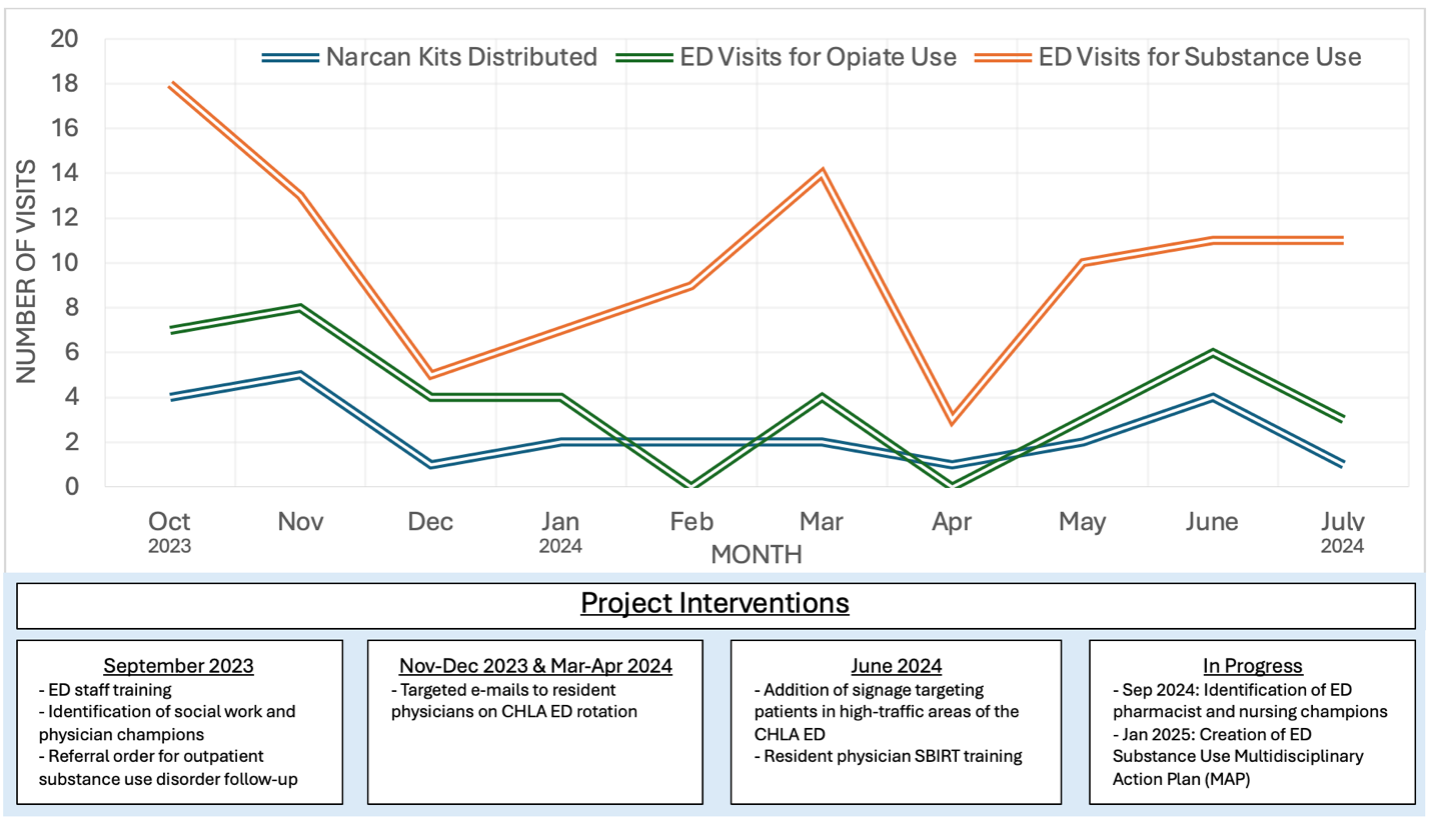
Figure 1. Example of an ‘opioid overdose kit’.
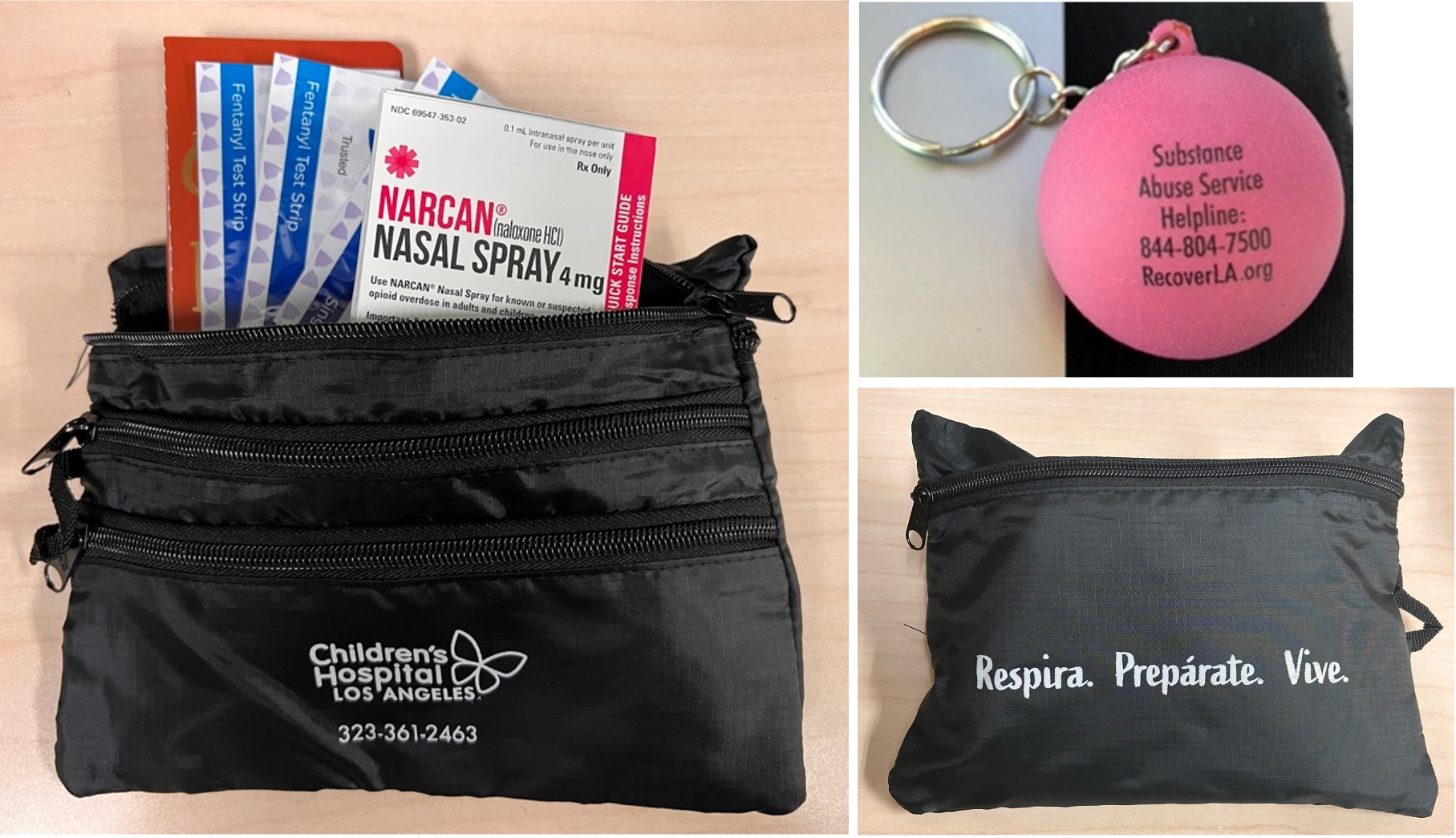 Naloxone kits included naloxone, fentanyl test strips, educational materials, and resources for outpatient substance use treatment. Kits were created in English, Spanish, Arabic, Armenian, Chinese, and Korean.
Naloxone kits included naloxone, fentanyl test strips, educational materials, and resources for outpatient substance use treatment. Kits were created in English, Spanish, Arabic, Armenian, Chinese, and Korean.Figure 2. Naloxone kit distribution compared to opiate and substance use monthly ED visits over time.