Emergency Medicine 4
Session: Emergency Medicine 4
252 - Pediatric Emergency Medicine Didactics and Simulation (PEMDAS): Armed Penetrating Trauma
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 252.5600
Amelia Wong, Monroe Carell Jr. Children's Hospital at Vanderbilt, nashville, TN, United States; Anita Thomas, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Jean I. Pearce, Medical College of Wisconsin, Milwaukee, WI, United States; Michael Levas, MCW, CIC, Project Ujima, Pewaukee, WI, 53072, WI, United States; Anita Bharath, Phoenix Children's Hospital, Phoenix, AZ, United States; Cecilia Monteilh, Phoenix Children's Hospital, Phoenix, AZ, United States; Rebecca Wilbur, Seattle Children’s Hospital, Seattle, WA, United States; Kimberly MacKeil-White, Monroe Carell Jr. Childrens Hospital Vanderbilt, Franklin, TN, United States; Daisy Ciener, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Elizabeth Sanseau, Children's Hospital of Philadelphia, Philadelphia, PA, United States

Amelia Wong, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Monroe Carell Jr. Children's Hospital at Vanderbilt
nashville, Tennessee, United States
Presenting Author(s)
Background: Firearms are the leading cause of pediatric death in the U.S, with increasing rates of firearm-related injuries presenting to Pediatric Emergency Departments (PED).1 Many healthcare workers have encountered firearms in the ED, despite a lack of workplace firearm handling training.
Objective: This simulation was developed to enhance pediatric emergency medicine (PEM) training in managing penetrating trauma and safe firearm handling in the ED.
Design/Methods: A high-fidelity simulation was developed for PEM trainees involving a 15-year-old male presenting with a gunshot wound (GSW) to the chest requiring needle decompression/chest tube placement and intubation. A concealed firearm discovered on the patient required proper handling protocols. Afterward a debrief was conducted and participants completed an evaluation based on pre- and post-simulation knowledge using a 5-point Likert scale (1 = Strongly Disagree, 5 = Strongly Agree).
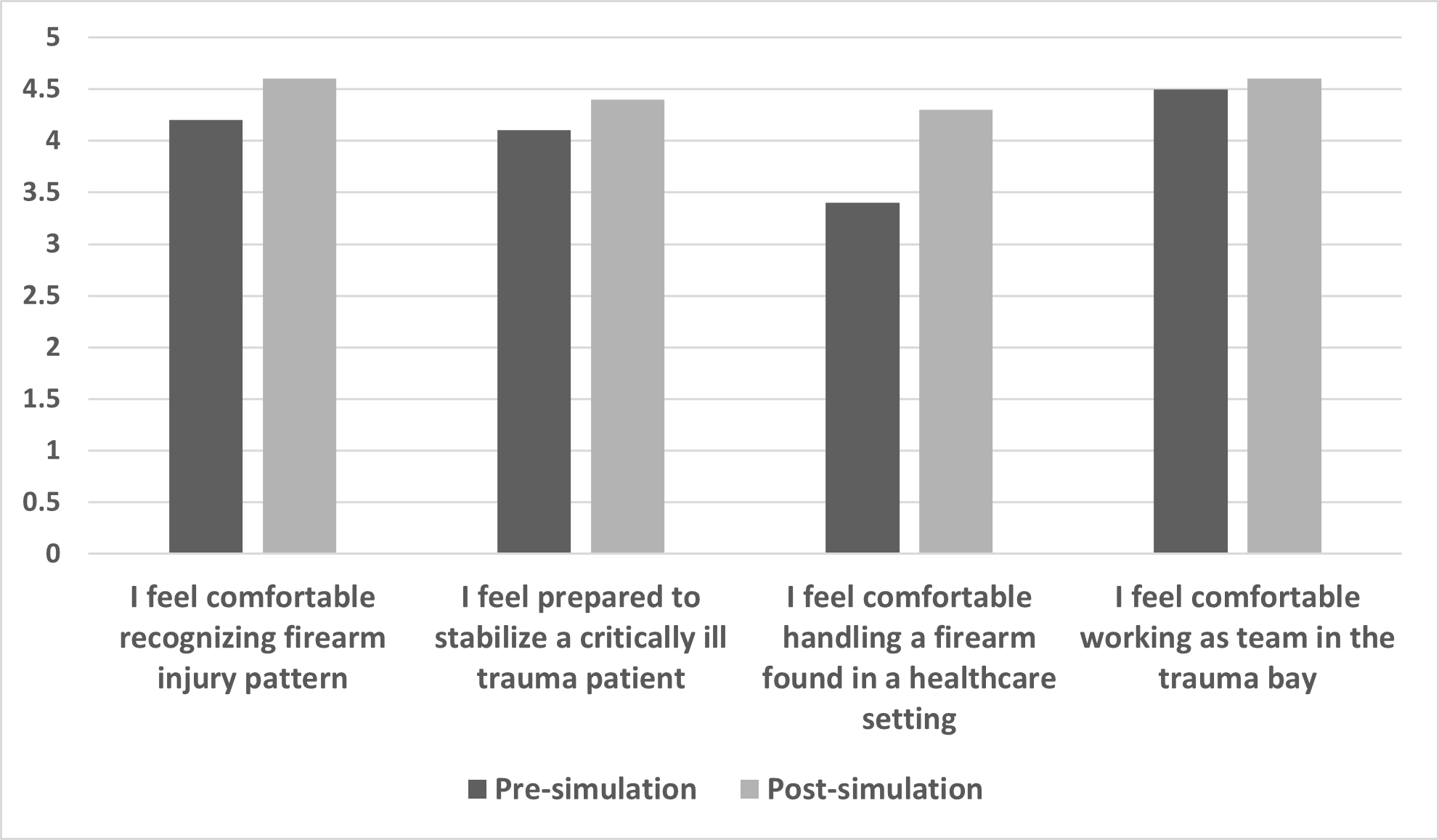
Results: There were 59 participants across four institutions. The simulation allowed the team to practice effective teamwork and communication skills (M = 4.6). Participants reported improved comfort recognizing firearm injury patterns (pre-simulation M = 4.2, post-simulation M = 4.6), preparedness to stabilize a critically ill trauma patient (pre-simulation M = 4.1, post-simulation M = 4.4), comfort in handling a firearm found in a healthcare setting (pre-simulation M = 3.4, post-simulation M = 4.3), and comfort working as team in the trauma bay (pre-simulation M = 4.5, post-simulation M = 4.6).
Conclusion(s): The simulation was well received, and participants found the simulation to be relevant (M = 4.8) and realistic (M = 4.7) while providing a psychologically safe environment. The simulation successfully improved participants' comfort and preparedness in managing GSWs and handling firearms encountered in the PED, as evidenced by positive feedback and self-reported gains in knowledge and confidence.
Table 1. Participant Cumulative Evaluation Scores (N = 59)
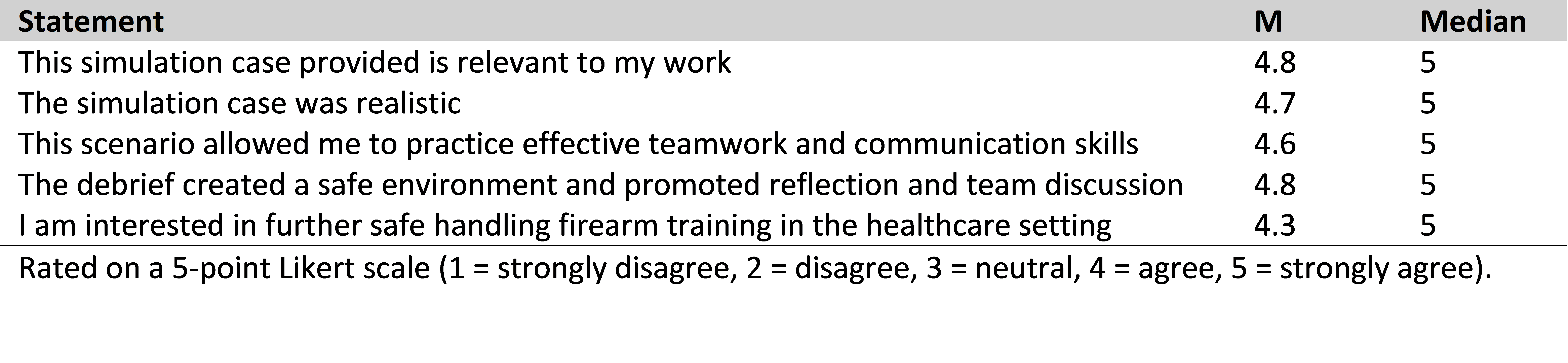
Figure 1. Pre-simulation and post-simulation evaluation scores (N = 59) rated on a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree).
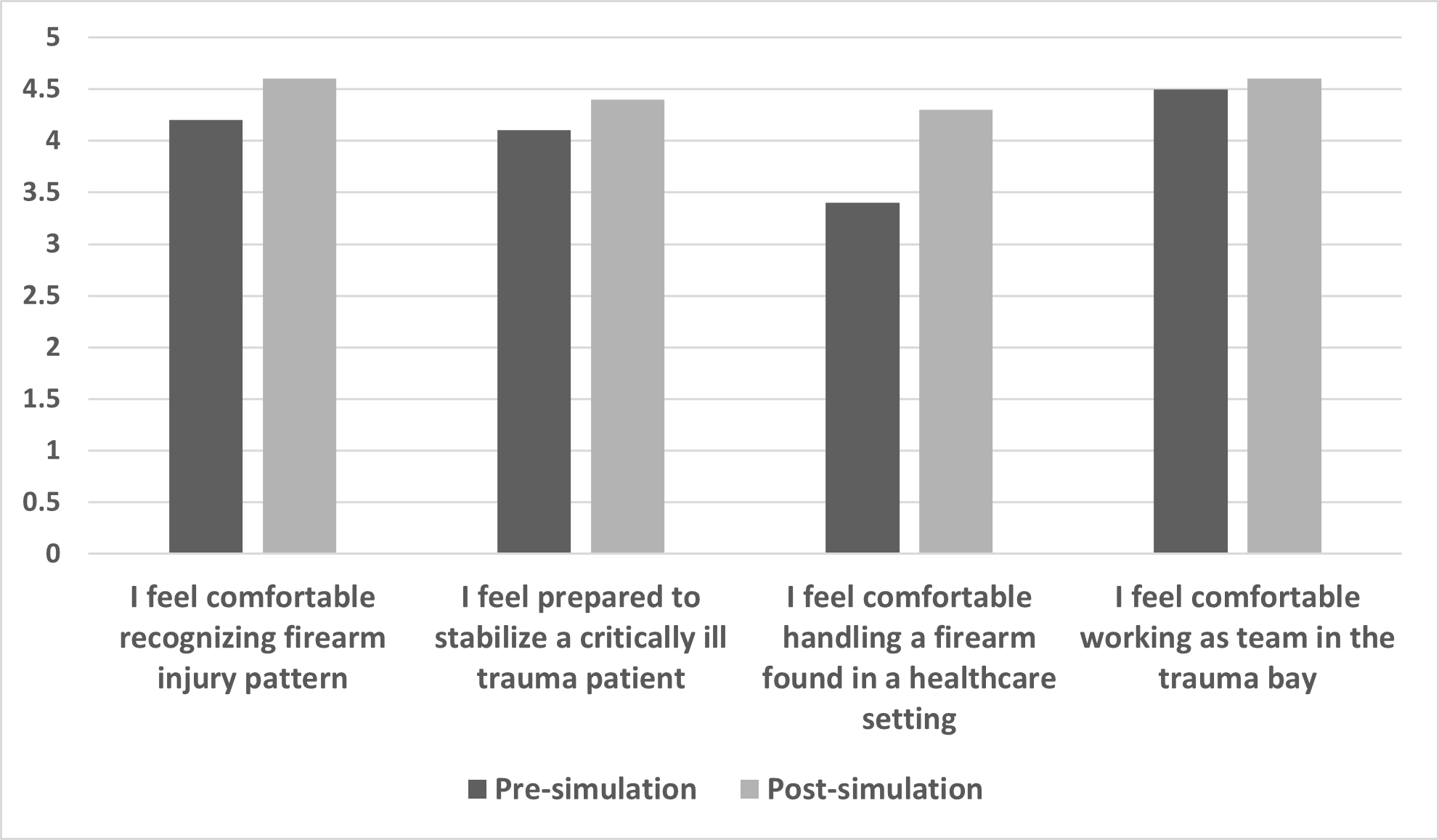
Table 1. Participant Cumulative Evaluation Scores (N = 59)
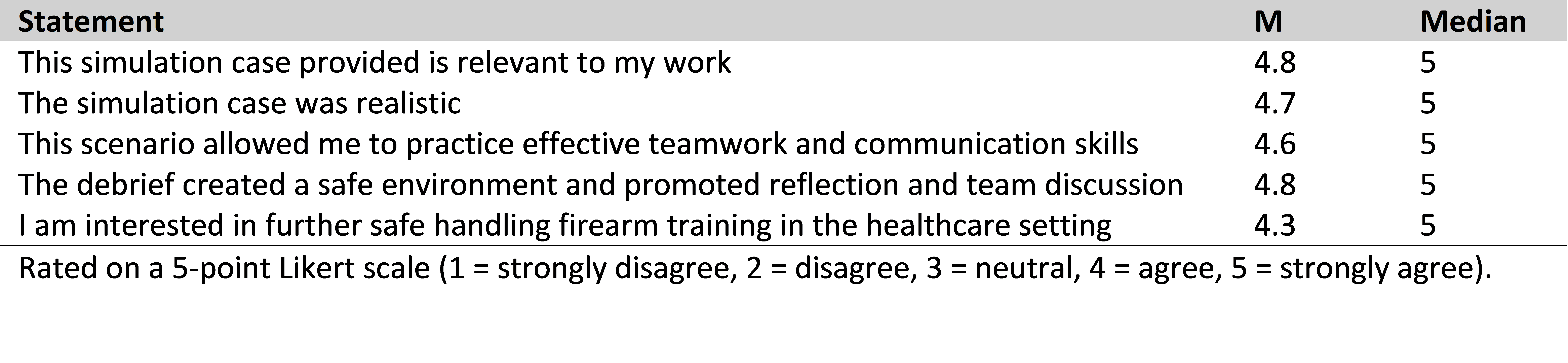
Figure 1. Pre-simulation and post-simulation evaluation scores (N = 59) rated on a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree).