Neonatal Hemodynamics and Cardiovascular Medicine 4
Session: Neonatal Hemodynamics and Cardiovascular Medicine 4
087 - Norepinephrine vs. Vasopressin for the Treatment of Hypotension among Neonates with Hypoxemic Respiratory Failure: A Retrospective Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 87.5598
Noor Shahab, Sunnybrook Health Sciences Centre, Toronto, ON, Canada; Sandra Gerges, Sunnybrook Health Sciences Centre, Toronto, ON, Canada; Nishkal Persad, University of Toronto Temerty Faculty of Medicine, Mississauga, ON, Canada; Alexander Kiss, Sunnybrook Research Institute/University of Toronto, Toronto, ON, Canada; Dany E. Weisz, University of Toronto, Toronto, ON, Canada

Sandra Gerges, PharmD, MSc
Clinical Pharmacist
Sunnybrook Health Sciences Centre
Toronto, Ontario, Canada
Presenting Author(s)
Background: Norepinephrine and vasopressin are commonly used vasopressors for the treatment of systemic hypotension among preterm and term neonates with acute pulmonary hypertension and hypoxemic respiratory failure (HRF) after birth. There is uncertainty regarding which agent is more effective in improving blood pressure and clinical outcomes.
Objective: This study aims to evaluate the association of norepinephrine vs. vasopressin and clinical outcomes among hypotensive neonates with HRF.
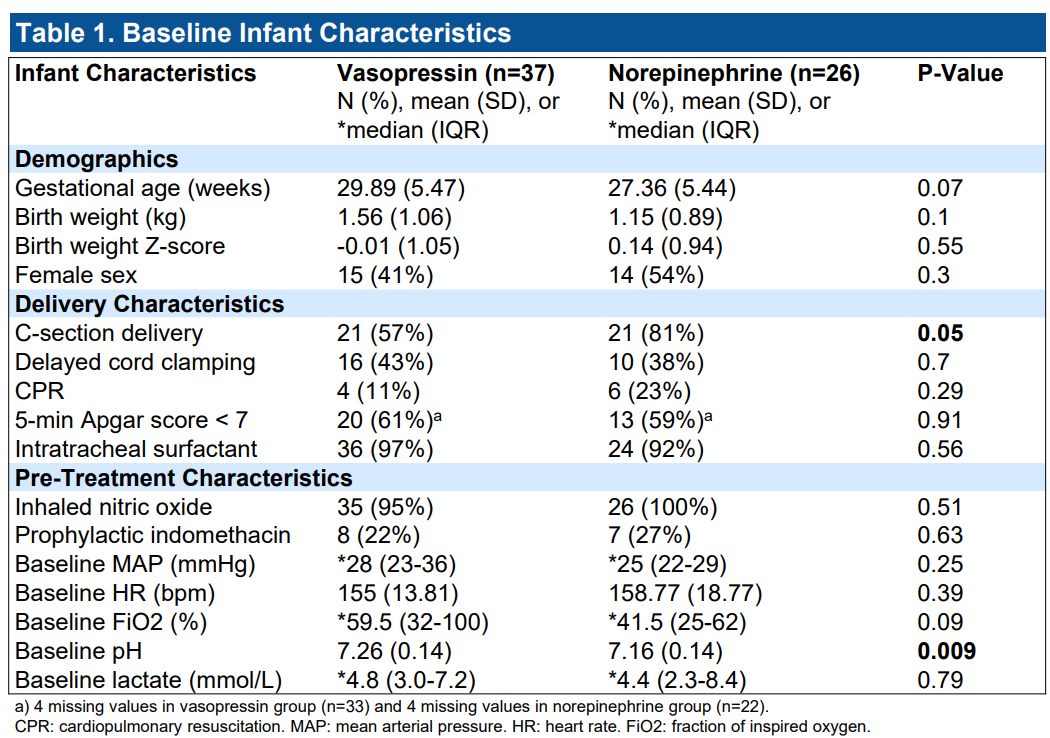
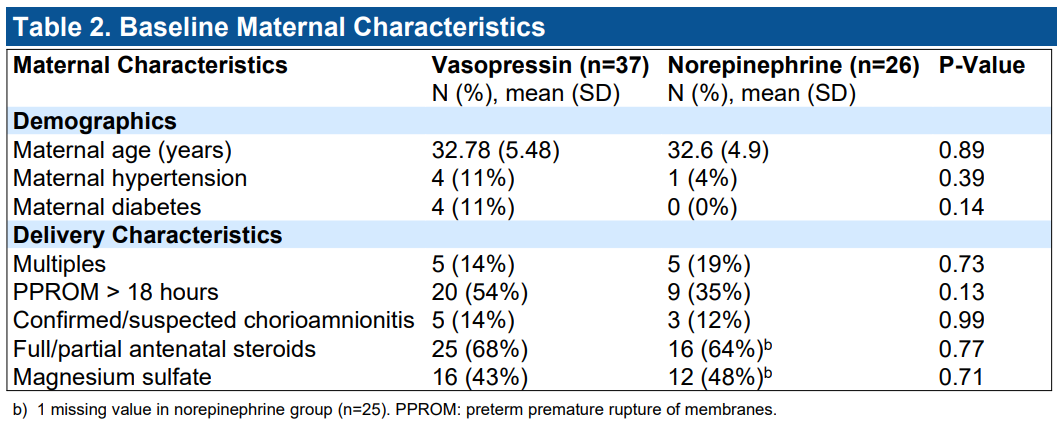
Design/Methods: We conducted a retrospective cohort study among preterm and term neonates with severe HRF and systemic hypotension, who required treatment with inhaled nitric oxide and/or had FiO2 requirements of ≥ 50%, and received norepinephrine or vasopressin treatment within 72 hours of birth. The primary outcome was treatment failure, defined as a composite of the need for additional vasopressor support or need to exceed the maximum conventional dose of the initial vasopressor. Secondary outcomes included mortality, necrotizing enterocolitis, severe intraventricular hemorrhage, and moderate-severe hyponatremia (defined as a serum sodium concentration ≤ 128 mEq/L). Multivariable logistic regression analysis was used to evaluate the association of vasopressor and clinical outcomes, adjusting for antenatal and perinatal confounders.
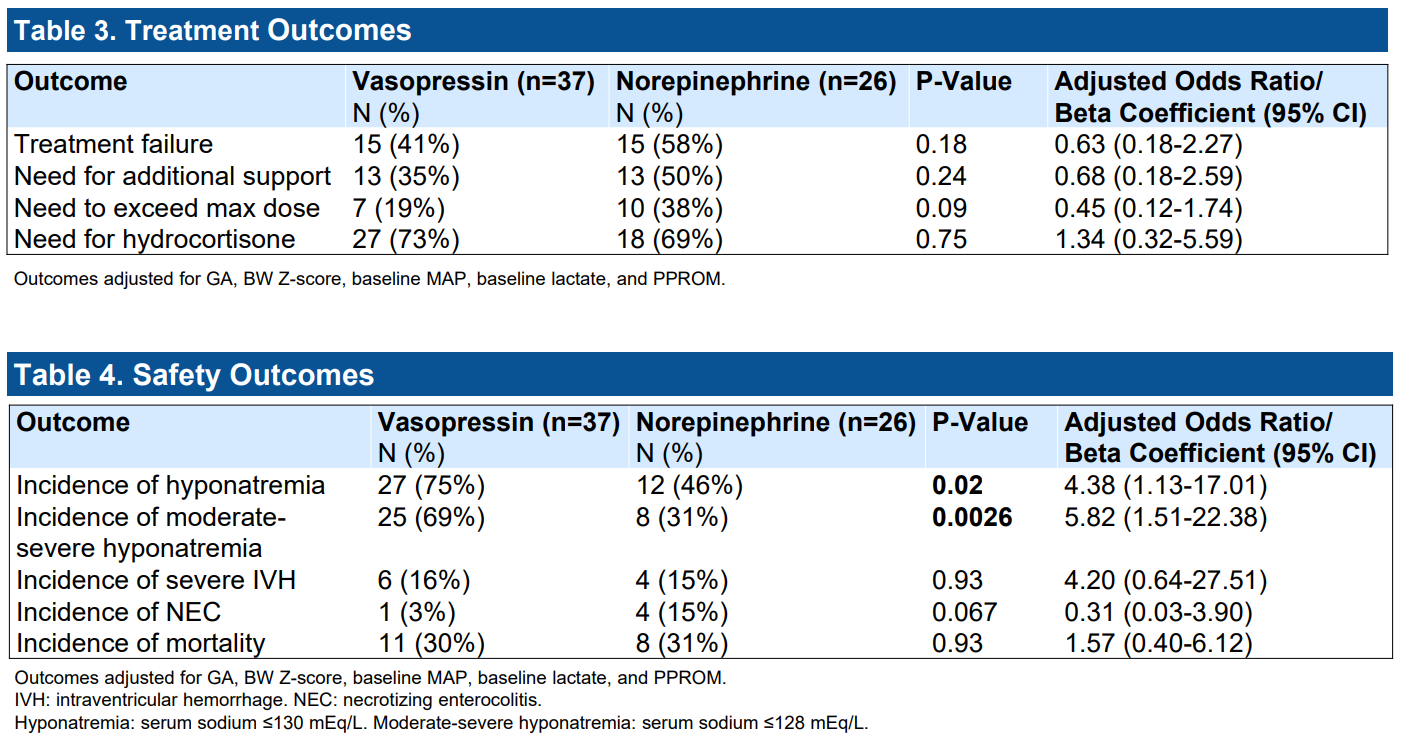
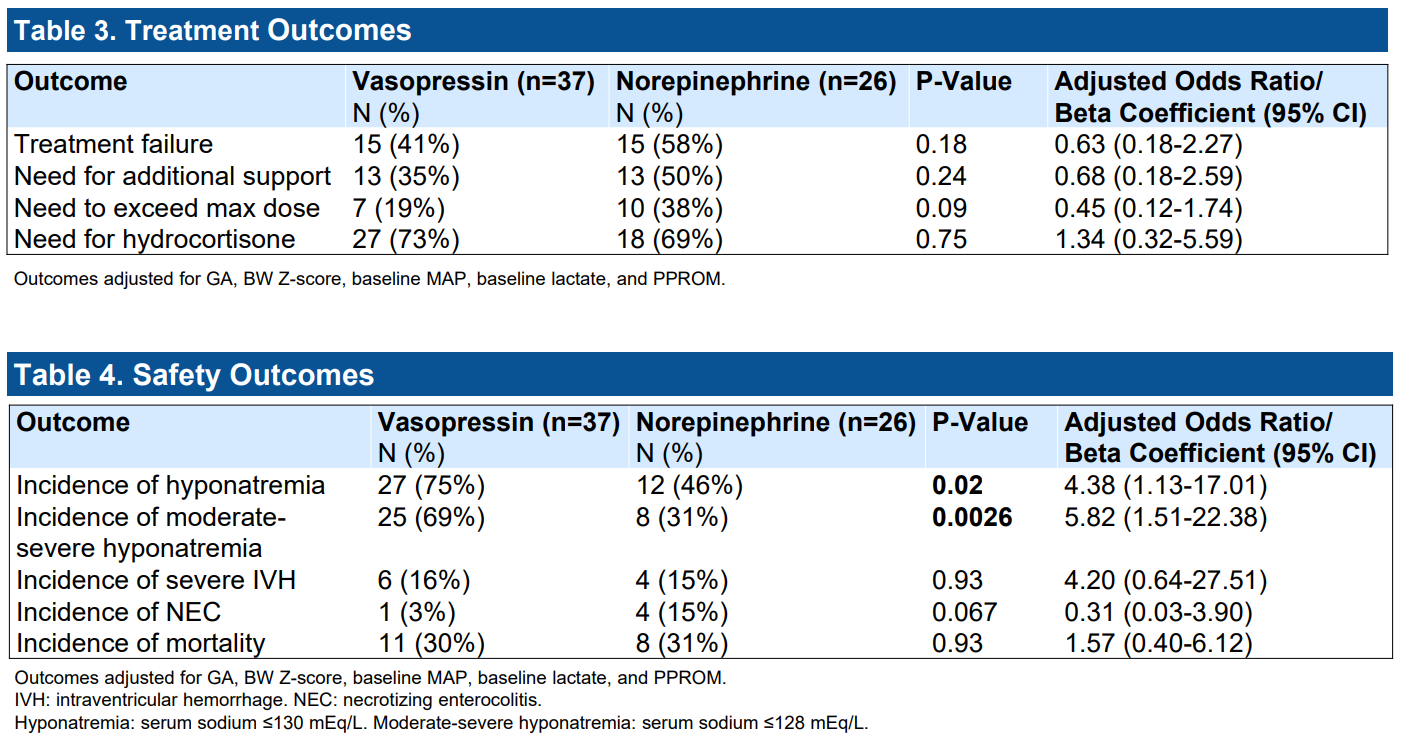
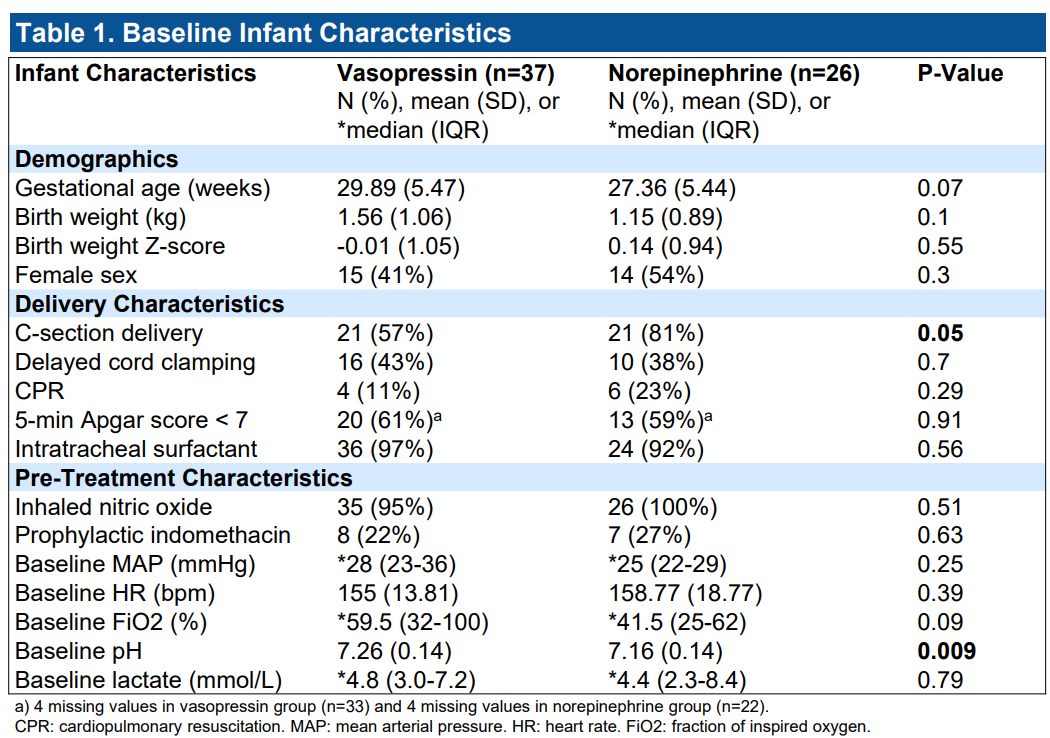
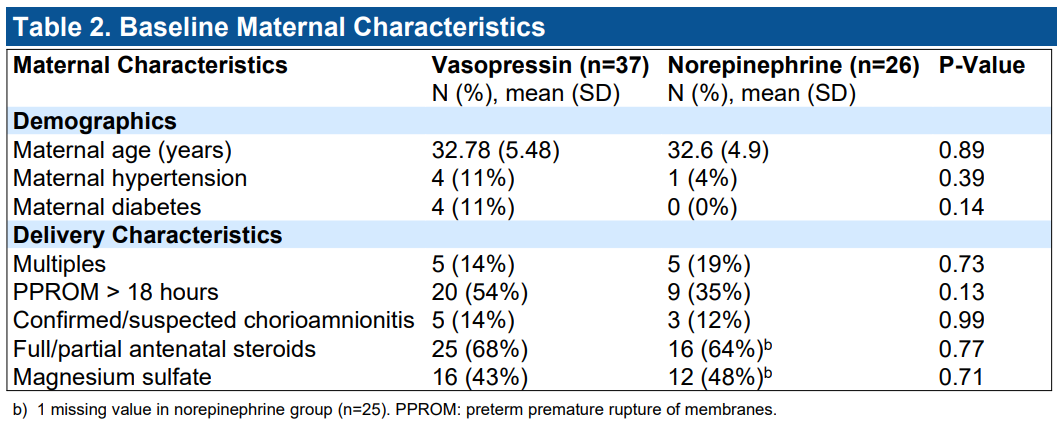
Results: Among 63 neonates (mean gestational age 28.8±5 weeks, mean birth weight 1.39±1.00 kg) with hypotension and severe HRF, 26 neonates were treated with norepinephrine and 37 with vasopressin. Compared to norepinephrine, treatment with vasopressin was not associated with an increase in treatment failure (aOR=0.63, 95% CI 0.18-2.27, p=0.18), the need for additional vasopressor support (aOR=0.68, 95% CI 0.18-2.59, p=0.24), the need to exceed the maximum conventional dose (aOR=0.45, 95% CI 0.12-1.74, p=0.09), mortality (aOR=1.57, 95% CI 0.40-6.12, p=0.93), necrotizing enterocolitis (aOR=0.31, 95% CI 0.03-3.90, p=0.067), or severe intraventricular hemorrhage (aOR=4.20, 95% CI 0.64-27.51, p=0.93). Neonates treated with vasopressin had a higher odds of developing moderate-severe hyponatremia (aOR=5.82, 95% CI 1.51-22.38, p=0.0026).
Conclusion(s): Among neonates with systemic hypotension and HRF, norepinephrine and vasopressin were associated with similar clinical outcomes; however, vasopressin treatment was associated with increased hyponatremia.
Baseline Infant Characteristics
Baseline Maternal Characteristics
Treatment and Safety Outcomes
Baseline Infant Characteristics
Baseline Maternal Characteristics
Treatment and Safety Outcomes