Neonatal Nephrology/AKI 1
Session: Neonatal Nephrology/AKI 1
009 - Neonatal Acute Kidney Injury and Neurodevelopmental Impairment: Investigating Associations in Very Low Birthweight Infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 9.5609
Jeffrey E. King, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Jill C.. Newman, Medical University of South Carolina College of Medicine, Mount Pleasant, SC, United States; Olivia Kinsinger, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Molly Mead, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Megan Rodgers, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Amy L. Ruddy-Humphries, MUSC, CHARLESTON, SC, United States; Cassandra Coleman, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; David Selewski, Medical University of South Carolina, Mount Pleasant, SC, United States; Heidi J.. Steflik, Medical University of South Carolina College of Medicine, Charleston, SC, United States

Jeffrey E. King, MD (he/him/his)
Fellow Physician
Medical University of South Carolina College of Medicine
Charleston, South Carolina, United States
Presenting Author(s)
Background: Associations between neonatal acute kidney injury (AKI) and neurodevelopmental impairment (NDI) remain understudied.
Objective: Investigate associations between AKI and NDI in very low birthweight (VLBW, < 1,500 grams at birth) infants. Hypothesis: In VLBW infants, AKI is associated with NDI.
Design/Methods: A single-center, retrospective cohort study of VLBW infants admitted to the Medical University of South Carolina (MUSC) Neonatal Intensive Care Unit (NICU) between 1/1/18-12/31/21 and evaluated in the MUSC NICU Developmental Clinic between 18 and 35 months of age. Neonatal AKI was diagnosed using the modified, neonatal Kidney Disease: Improving Global Outcomes (KDIGO) serum creatinine criteria. NDI was a composite primary outcome, defined as one or more of the following: hearing impairment or a developmental quotient (DQ, i.e., age-equivalent level of function divided by the adjusted gestational age, multiplied by 100) < 75% on the Cognitive Adaptive Test (CAT), Clinical Linguistic and Auditory Milestone Scale (CLAMS), and/or Modified Peabody Developmental Motor Scale (PDMS-M). Descriptive statistics were examined overall and by AKI status. Bivariate and multivariable generalized linear mixed modeling was used to examine associations between AKI and NDI.
Results: Of 203 infants included, 64 (32%) experienced neonatal AKI and 76 (37%) developed NDI. Differences noted in those with AKI, compared to those without, included lower birth weight (BW; AKI: 829 ± 211 grams vs no AKI: 1,110 ± 259 grams), younger gestational age (GA; 26.0 ± 2.1 weeks’ vs 28.8 ± 2.3 weeks’), less maternal pre-eclampsia (27% vs 44%), more supplemental oxygen at discharge (40% vs 13%), and increased length of stay (LOS; 110 [89,128] days vs 65 [40,90] days) (all p< 0.02). Similar findings were noted in those with NDI compared to those without (BW: NDI: 911 ± 252 grams vs no NDI: 1,087 ± 271 grams, GA: 27.1 ± 2.8 weeks’ vs 28.4 ± 2.4 weeks’, maternal pre-eclampsia: 24% vs 47%, supplemental oxygen at discharge: 33% vs 14%, and LOS: 93 [68,120] days vs 68 [43,100] days (all p< 0.01)).
The relative risk of NDI was significantly higher in those with AKI (Table 1). Examining associations between AKI and each component of the NDI composite detected an increased risk of CLAMS and PDMS-M DQ < 75% in those with AKI (Table 1). In multivariable analysis, AKI was not an independent predictor of NDI (Table 2).
Conclusion(s): In bivariate analyses, AKI was a significant predictor of NDI driven by language and motor delays. In a multivariable model, AKI was no longer an independent predictor of NDI. Further investigation is warranted.
Study Participants
.png)
Table 1: Associations between Acute Kidney Injury and Neurodevelopmental Impairment
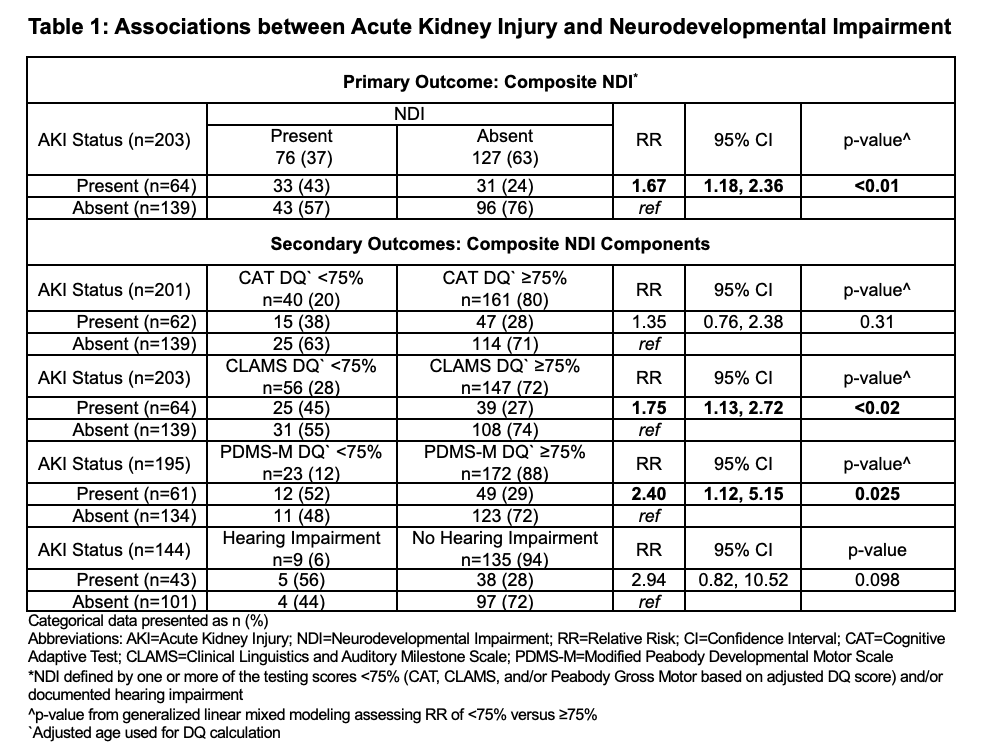
Table 2: Bivariate and Multivariable Associations between Acute Kidney Injury and Neurodevelopmental Impairment
.png)
Study Participants
.png)
Table 1: Associations between Acute Kidney Injury and Neurodevelopmental Impairment
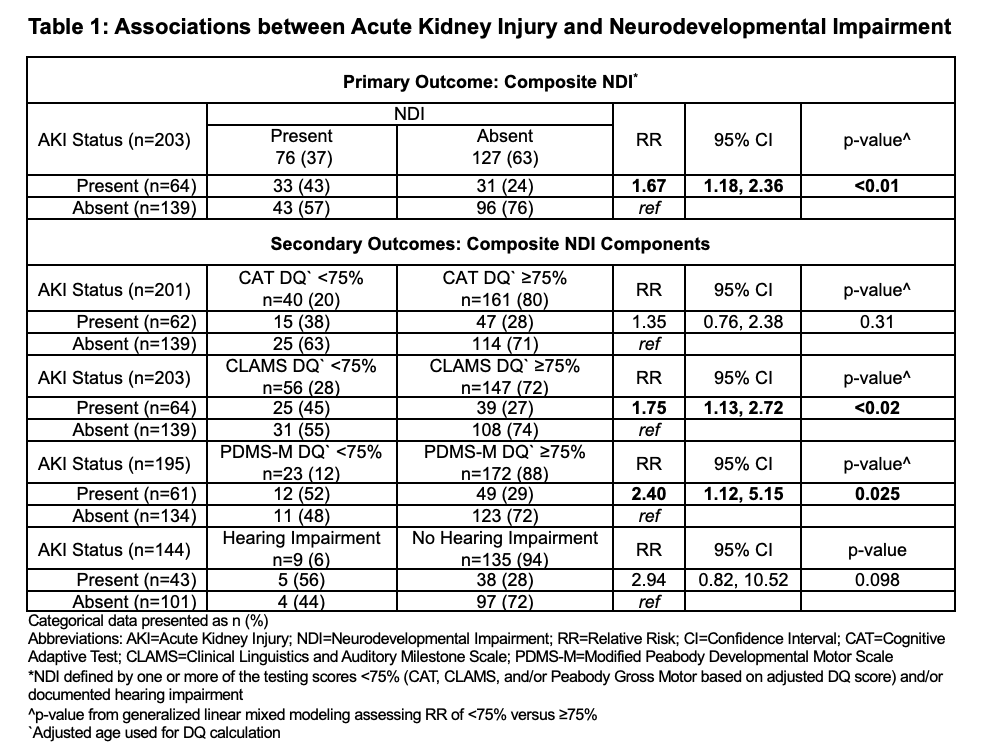
Table 2: Bivariate and Multivariable Associations between Acute Kidney Injury and Neurodevelopmental Impairment
.png)

