Emergency Medicine 5
Session: Emergency Medicine 5
265 - Multidisciplinary Timely Debrief Sessions After Cardiac Arrests and Endotracheal Intubations in the Pediatric Emergency Department
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 265.5644
Jonathan A. Hermel, UC San Diego and Rady Children's Hospital, San Diego, CA, United States; Yvette Wang, Rady Children's Hospital San Diego, San Diego, CA, United States; Martha Pannepacker, Rady Children's Hospital San Diego, San Diego, CA, United States; Daniel Roderick, Rady Children's Hospital San Diego, San Diego, CA, United States; Jillian Berman, Rady Children's Hospital San Diego, San Diego, CA, United States; Elise Zimmerman, Rady Children's Hospital San Diego, San Diego, CA, United States

Jonathan A. Hermel, MD (he/him/his)
Resident Physician
UC San Diego and Rady Children's Hospital
San Diego, California, United States
Presenting Author(s)
Background: Multidisciplinary clinical debriefs are formal team discussions after critical events intended to assess performance, identify areas for improvement, and provide staff support. Debriefs enhance team performance and well-being but are underutilized in high-acuity settings. We identified a need to establish standardized debriefing protocols after critical pediatric emergency department (ED) incidents to foster continuous improvement and resilience in health care providers.
Objective: Our aim was to increase debriefs after ED critical events (cardiac arrests and endotracheal intubations) from 4% to 50% within 9 months. The outcome measure was the percentage of critical events with a debrief completed and documented. To assess if debriefs hindered ED workflow, our balancing measure was room-to-provider times for all emergency severity index (ESI) level 1 and 2 patients.
Design/Methods: We created a key driver diagram to identify drivers and interventions (Fig. 1). Using a validated plus-delta improvement framework, we developed a standardized REDCap form to document each debrief. Quick response (QR) codes posted throughout the ED provided access to this form (Fig. 2). Debriefs occurred within 30 minutes after the event, lasting up to 7 minutes. We conducted Plan-Do-Study-Act cycles with educational interventions, including staff meeting presentations, newsletters, email reminders, and ED signs, as well as designated quality improvement champions. Debrief use was assessed as the percentage of critical incidents with a completed form. We used statistical process control to examine changes in measures over time.
Results: We achieved special cause variation, observing a 9.3-fold increase in the percentage of completed debriefs. Although we did not achieve our goal, we increased debriefs after critical events from a baseline of 4% to 41% (Fig. 3). Mean room-to-provider time for ESI level 1 and 2 patients remained unchanged.
Conclusion(s): We markedly increased the percentage of standardized debriefs completed after ED critical events without affecting room-to-provider times for high-acuity patients. This confirms the feasibility of integrating rapid, structured debriefs in a high-acuity ED, underscoring the potential for ongoing improvement through continued education and team engagement. Future efforts will focus on increasing participation and evaluating the impact on team performance and well-being.
Figure 1: Key Driver Diagram
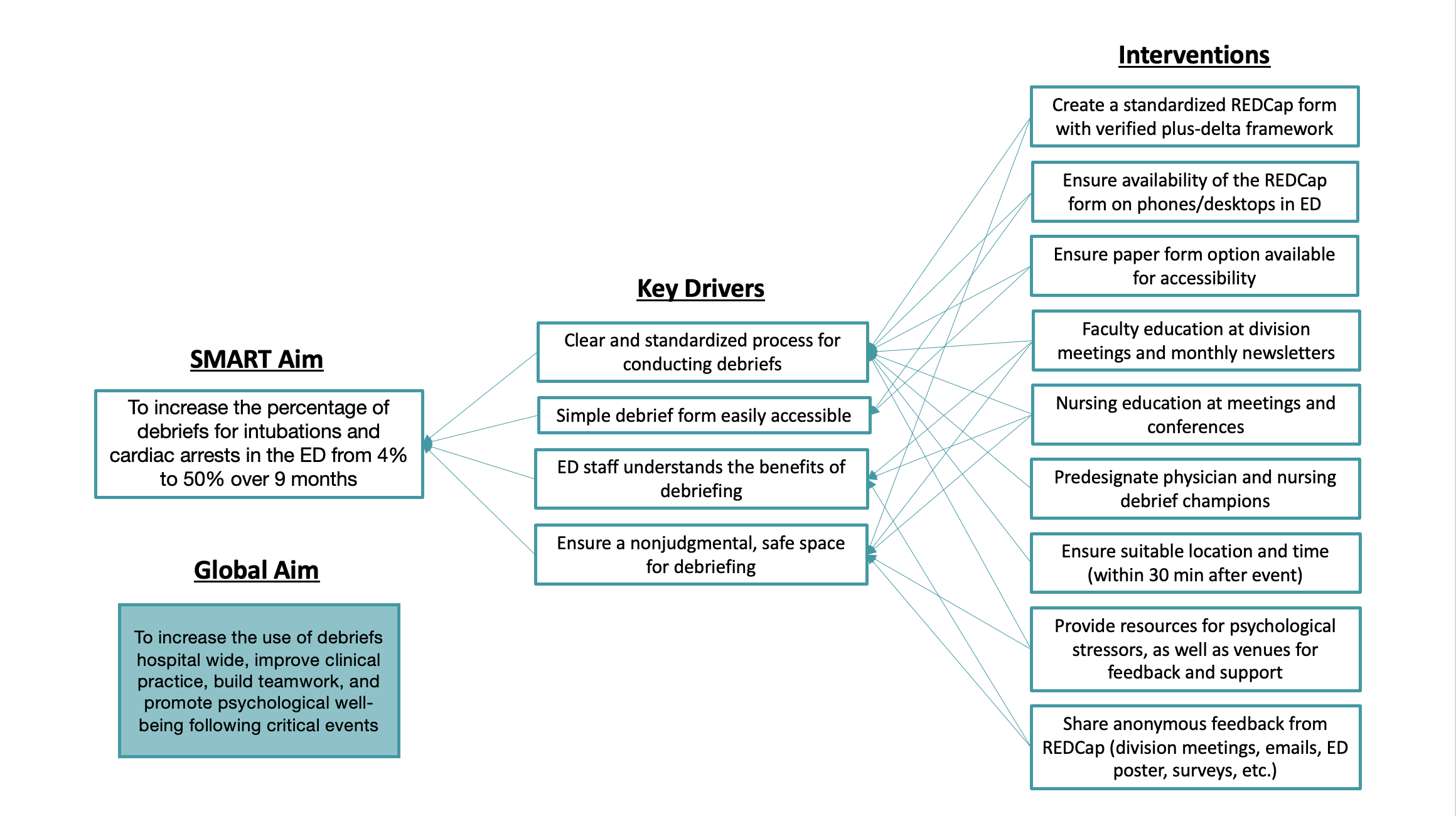
Figure 2: QR Code
.png) REDCap Debrief Form
REDCap Debrief FormFigure 3: Statistical Process Control Chart
.png)
Figure 1: Key Driver Diagram
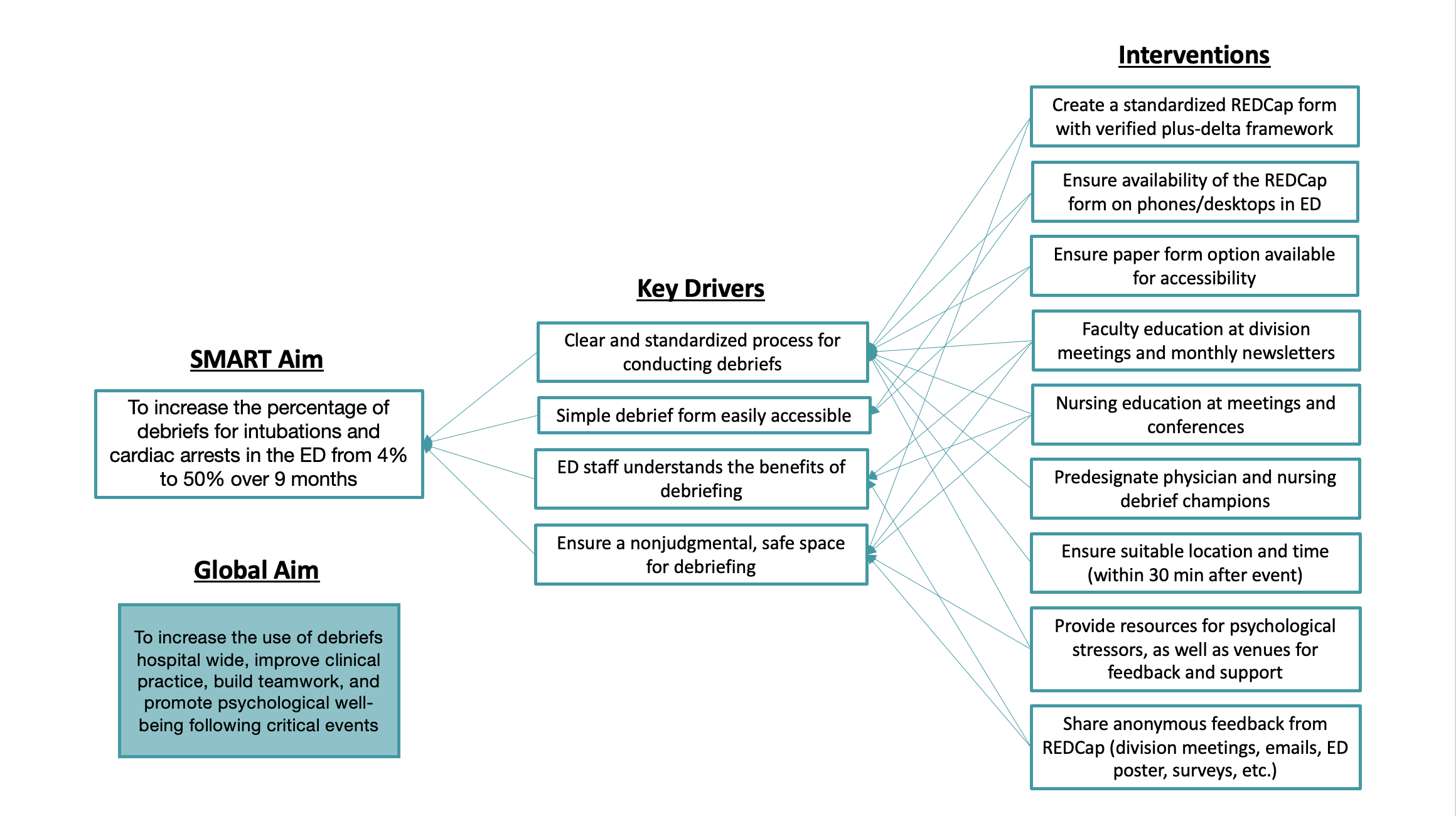
Figure 2: QR Code
.png) REDCap Debrief Form
REDCap Debrief FormFigure 3: Statistical Process Control Chart
.png)


