Mental Health 1
Session: Mental Health 1
760 - Mental Health INtegration and Development (MIND) in Primary Care Pediatrics
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 760.5879
Kelly Chiu, Harvard Medical School, Belmont, MA, United States; Caroline N. Breen, Boston Children's Hospital, CAMBRIDGE, MA, United States; Katherine Barahona Paz, Boston Children's Hospital, Cambridge, MA, United States; Olivia Carrick, Boston Children's Hospital, Boston, MA, United States; Alexandra Epee-Bounya, Boston Children's Hospital, boston, MA, United States
- KC
Kelly Chiu, MD (she/her/hers)
Assistant Professor
Harvard Medical School
Belmont, Massachusetts, United States
Presenting Author(s)
Background: Children and teens in the US are in a mental health crisis and primary care pediatricians are on the frontlines. Nearly 1 in 5 children have a mental, emotional, or behavioral disorder (e.g., ADHD, anxiety, autism spectrum disorder), and only about 20% of these children receive care from a specialized mental health provider. Long wait times and stigma around Behavioral Health are barriers to accessing needed services. The AAP recommends that primary care pediatricians (PCPs) manage mild-moderate behavioral health (BH) concerns. However, primary care providers report feeling unprepared to address behavioral health (BH) concerns. Only 1 in 3 pediatricians report they have adequate training. They are also facing time constraints that limit their ability to address BH concerns.
Objective: To promote behavioral health equity in Primary Care through a dedicated Mental health INtegration and Development (MIND) clinic.
Design/Methods: At an urban health care center, care is provided for more than 7,300 patients aged 0 to 27. 85% of patients have public insurance and 49% have a preferred language other than English. A primary care pediatrician completed additional training in developmental and behavioral pediatrics in 2023, focused on autism spectrum disorder (ASD) and complex ADHD (Figure 1). The MIND pediatrician receives referrals from other PCPs and offers a telemedicine visit to manage mental, behavioral, developmental, and psychopharmacology concerns. They collaborate with on-site social work and psychiatry as needed. High-acuity patients post-psychiatric admission also meet with this provider until the patient can see a psychiatrist. Patient demographics, referral and follow-up dates, screening, and medications were tracked and collected by the study team.
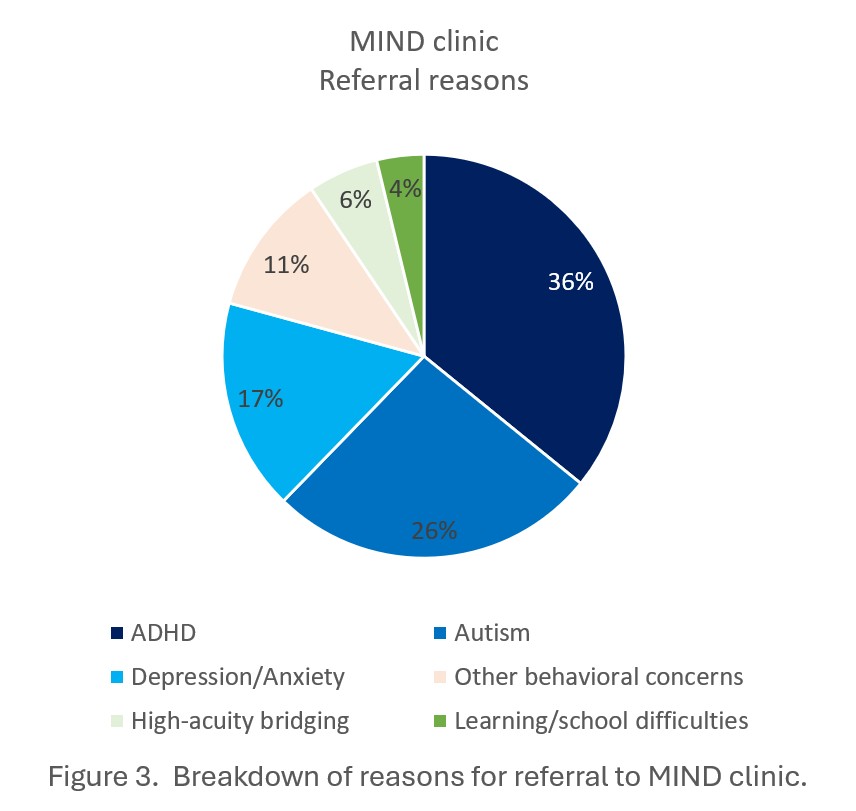
Results: From May 2023 – Oct 2024, the provider received more than 70 referrals from MEHC providers and saw 53 patients at the MIND clinic, with 15 (28%) completing at least one follow-up visit so far. The average time from referral to appointment in the MIND clinic is 32 days compared to 96 days in psychiatry (Figure 2). 9 (17%) of the 53 patients had appointments completed in a language other than English (7 Spanish, 1 Portuguese, and 1 Cape Verdean). 36% of all referrals were for ADHD concerns, 26% for ASD concerns, the remaining 38% were for depression/anxiety, high-acuity bridging, learning/school difficulties, or other (Figure 3).
Conclusion(s): The MIND clinic is an alternative model of behavioral health care delivery in primary care setting for mild-moderate BH concerns that can increase access to behavioral health care.
Figure 1. Driver Diagram displaying the goal of reducing wait times for behavioral health (BH) support along with key drivers, general and MIND specific interventions.
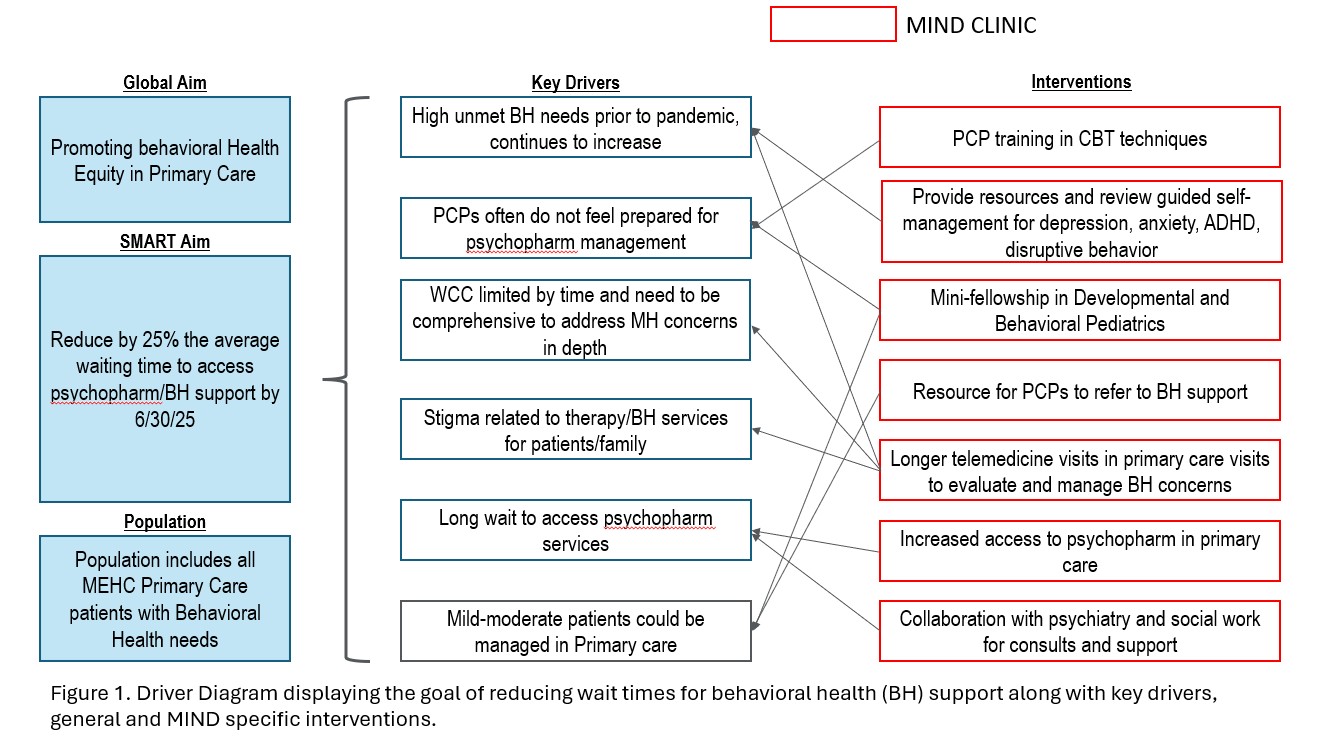
Figure 2. Average quarterly time to first appointment with psychopharmacology or MIND clinic provider.
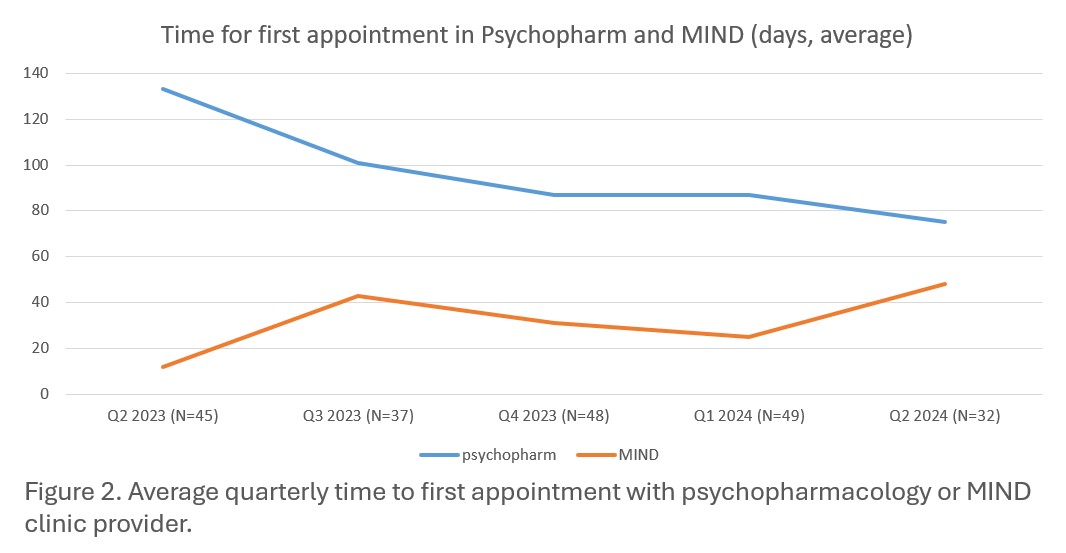
Figure 3. Breakdown of reasons for referral to MIND clinic