Clinical Bioethics
Session: Clinical Bioethics
583 - Parental Experiences of Decision-Making in the Grey Zones of Neonatal Intensive Care: An International Multi-Centre Mixed Methodology Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 583.5851
Trisha M. Prentice, The Royal Children's Hospital, Melbourne, Victoria, Australia; Gillian W. Foo, Western Health, Melbourne, Victoria, Australia; Natalie Jewitt, The Hospital for Sick Children, Toronto, ON, Canada; Jack Turley, Monash Children’s Hospital, Melbourne, Victoria, Australia; Joseph Kates Rose, Children's Hospital of Eastern Ontario, University of Ottawa, Ottawa, ON, Canada; Michelle L. Stoopler, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Bianca M. Bartholomew, Monash Health, Bayswater, Victoria, Australia; Christopher Tomlinson, The Hospital for Sick Children, Toronto, ON, Canada; Rebecca Greenberg, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Gregory P. Moore, CHEO, Ottawa, ON, Canada

Trisha M. Prentice, MBBS BMedSci MBioeth FRACP PhD (she/her/hers)
Neonatologist
The Royal Children's Hospital
Melbourne, Victoria, Australia
Presenting Author(s)
Background: Shared decision-making (SDM) with parents in the NICU is complex. In grey zones (where multiple morally acceptable decisions are possible) it is not uncommon for families and clinicians to disagree about the best path forward. Moral distress (MoD) is well recognised in clinicians, yet little is known about parental moral experiences of decision making (DM).
Objective: To understand parental experiences of end-of-life DM in the NICU. In particular, whether the concepts of moral schism and MoD were experienced, in four NICUs in Australia and Canada.
Design/Methods: This was a mixed-methodology phenomenological study. Parents of infants who were admitted for 3 or more days between July 2018 and August 2022 and who engaged in end-of-life conversations were invited to complete a survey that sought their experiences of DM. Bereaved families were not contacted until 1 year had passed following the death of their child. Patient data was collected by retrospective chart review. Qualitative data was analysed using thematic analysis, informed by the concepts of moral distress and moral schism. Descriptive statistics were used for quantitative data.
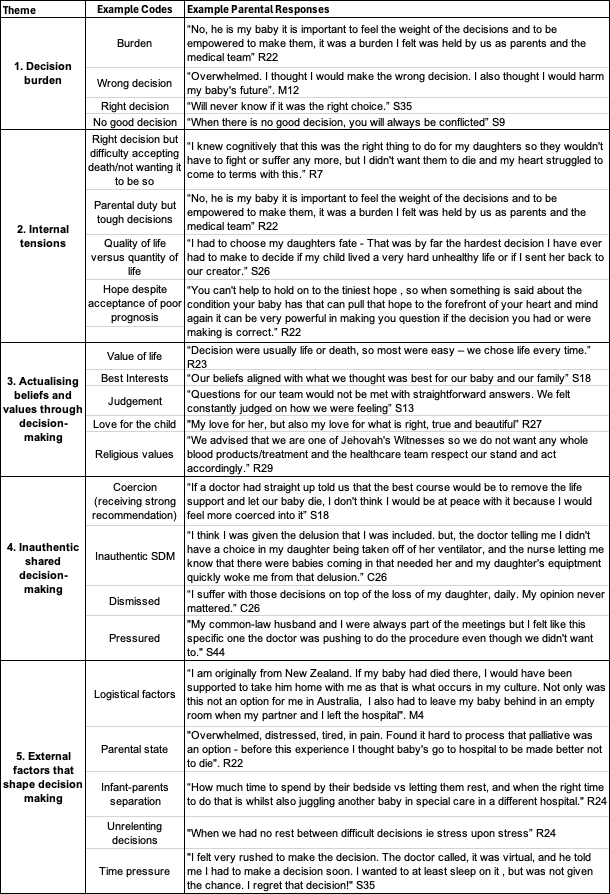
Results: 71 parents (80% mothers) completed the survey. Thematic analysis revealed 5 main themes: (1) decision burdens, (2) internal tensions, (3) actualising beliefs and values through DM, (4) inauthentic SDM and (5) external factors that shaped decision-making. (See table 1). Parents reported variable experiences of SDM. Despite DM commonly being described as burdensome, 89% wanted to be involved in SDM; and 63% felt included. While parents valued actualisation of their beliefs and values, views on who should be the ultimate decision-makers in end-of-life decisions varied significantly. Time pressures, frequency of DM, competing interests, and environmental factors positively and negatively added to the internal tensions experienced. Despite being framed as SDM, some parents felt coerced into decisions, consistent with moral distress. The inability to advocate for their child in alignment with their values was a source of regret for some.
Conclusion(s): SDM dynamics are complex, reflecting the need for personalised DM. Parents found the weight of DM burdensome, but wanted to be involved. Enacting SDM requires clinicians to be aware of various external and internal pressures and tensions experienced by some parents. A nuanced approach should mitigate negative moral experiences during DM in clinicians and families alike.
Table 1: Thematic analysis of parental responses