Emergency Medicine 6
Session: Emergency Medicine 6
286 - Reducing Antibiotic Duration for Pneumonia and Sinusitis in the Emergency Department: A Quality Improvement Approach
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 286.6107
Joshua A. Saucedo, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Leslie Ann. Hueschen, Children's Mercy Hospitals and Clinics, KANSAS CITY, MO, United States; Amanda Nedved, Children's Mercy, Lenexa, KS, United States; Marsha Dannenberg, Children's Mercy Hospitals and Clinics, Overland Park, KS, United States; PATRicia A. Phillips, Childrens Mercy Kansas, Raymore, MO, United States; Jen Floyd, Children's Mercy Hospitals and Clinics, Overland Park, KS, United States; Alaina Burns, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Rana E. El Feghaly, Children's, Kansas City, MO, United States

Joshua A. Saucedo, MD (he/him/his)
Pediatric Emergency Medicine Fellow
Children's Mercy Hospitals and Clinics
Kansas City, Missouri, United States
Presenting Author(s)
Background: Limiting antibiotic duration is one of the pillars of antimicrobial stewardship programs (ASP) as it reduces unnecessary antibiotic exposure. In our emergency department (ED), >90% of respiratory infections are treated with first-line guideline-recommended antibiotics, however, duration continues to be prolonged especially for community acquired pneumonia (CAP) and acute bacterial rhinosinusitis (ABRS). National guidelines recommend shortening antibiotic durations to 3-5 days for CAP and 5-7 days for ABRS, however only 22% of discharged ED patients receive the recommended duration.
Objective: Our aim is to increase the percentage of children discharged home from the ED with a diagnosis of CAP or ABRS treated with an optimal antibiotic duration (3-5 days for CAP, 5-7 days for ABRS) from 22% to 70% by July 2025.
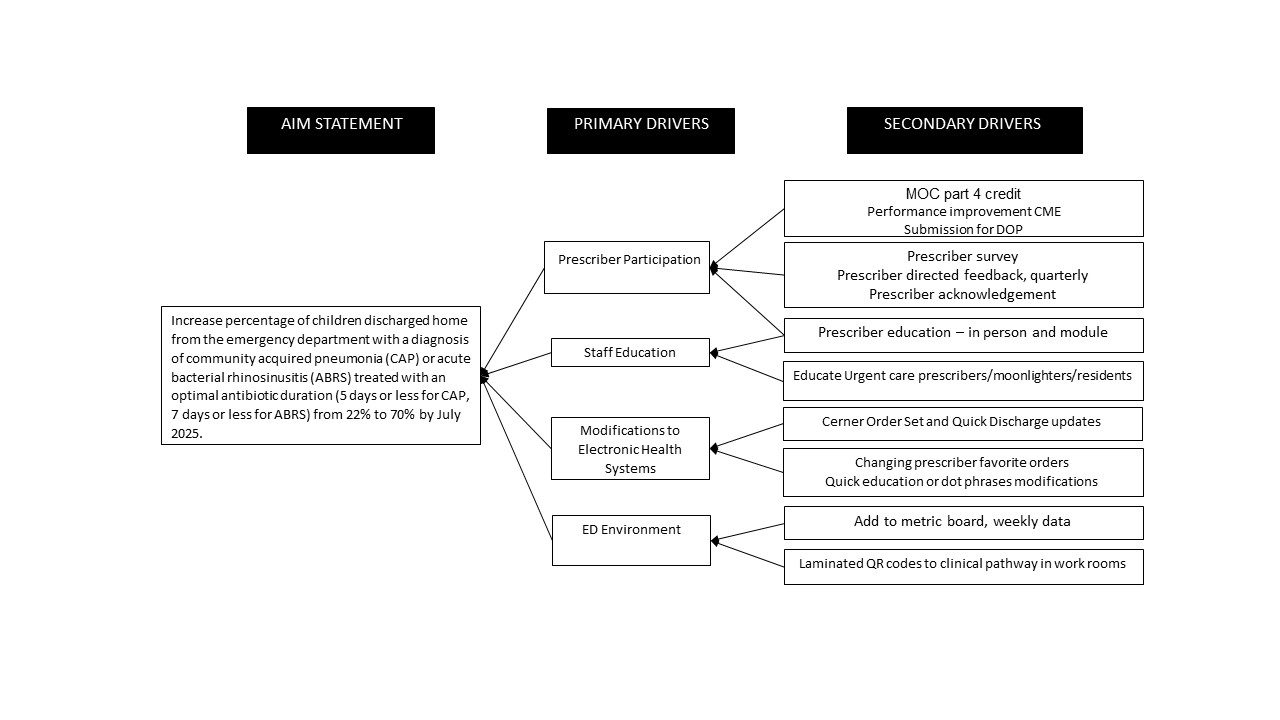
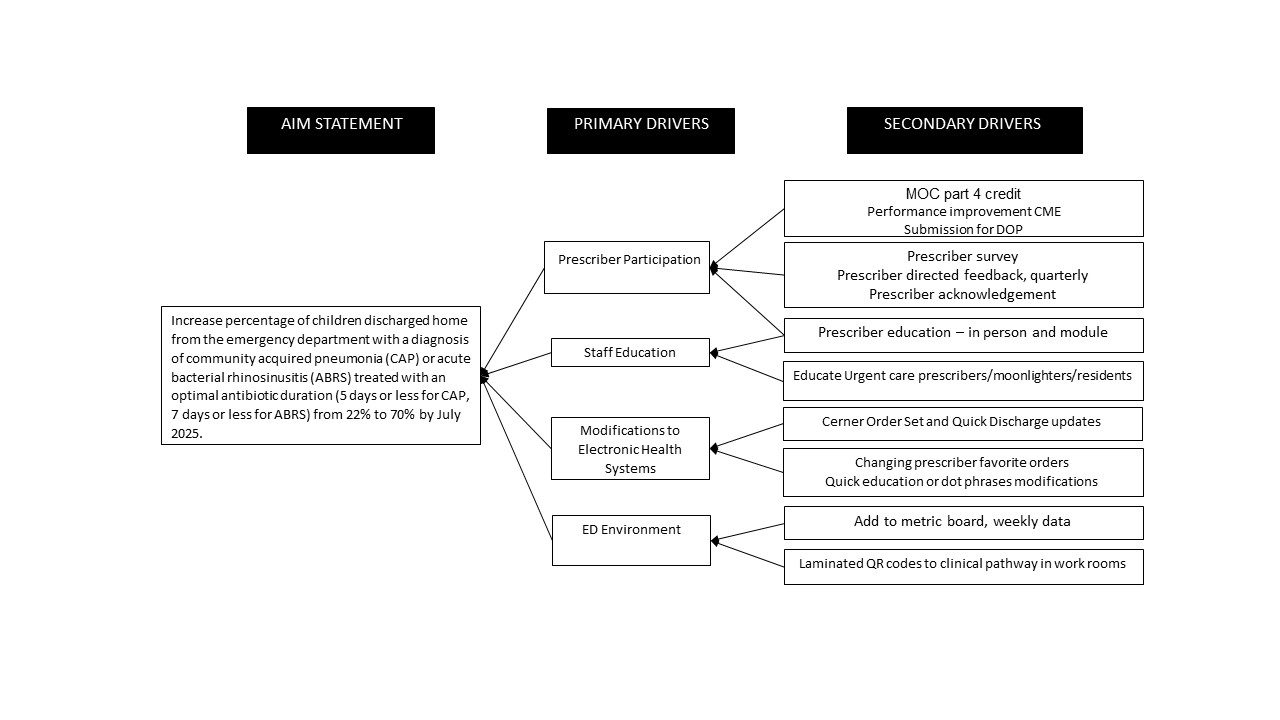
Design/Methods: Outcome metric is the percentage of patients receiving recommended antibiotic duration for CAP and ABRS. Process metrics include use of order set, "Quick Discharge” order set, and clinical pathway QR codes. Balancing metric is the number of return visits with the same diagnosis < 14 days. Plan-Do-Study-Act methodology was used. In August 2023, our robust ASP program disseminated a handbook that emphasized these shorter durations. A new multidisciplinary team (infectious diseases, ED, and urgent care physicians, advanced practice providers, nurses, and pharmacy) formed in December 2023. We utilized cause-and-effect analysis, driver diagram (Figure 1), and prioritization matrix (Figure 2), which helped identify other impactful interventions, including implementation of new internal CAP clinical pathway order set (April 2024) and “Quick Discharge” order sets (May 2024). Next, we surveyed prescriber comfort (June 2024) with shorter duration identifying barriers and providing education, which has led to posting evidence for lower duration treatment in provider workrooms and developing a new ABRS clinical pathway (September 2024).
Results: We saw shifts in the outcome metric’s center line in September 2023 and May 2024 to 59.0% with no change in balancing metric (Figures 3A-C).
Conclusion(s): We saw a reduction in antibiotic durations for CAP and ABRS with development of standard order set and discharge through the electronic medical record and prescriber education interventions. Future PDSA cycles will focus on barrier mitigation, increased data transparency, with huddle board reminders and prescriber acknowledgements.
Key Driver Diagram
Prioritization Matrix
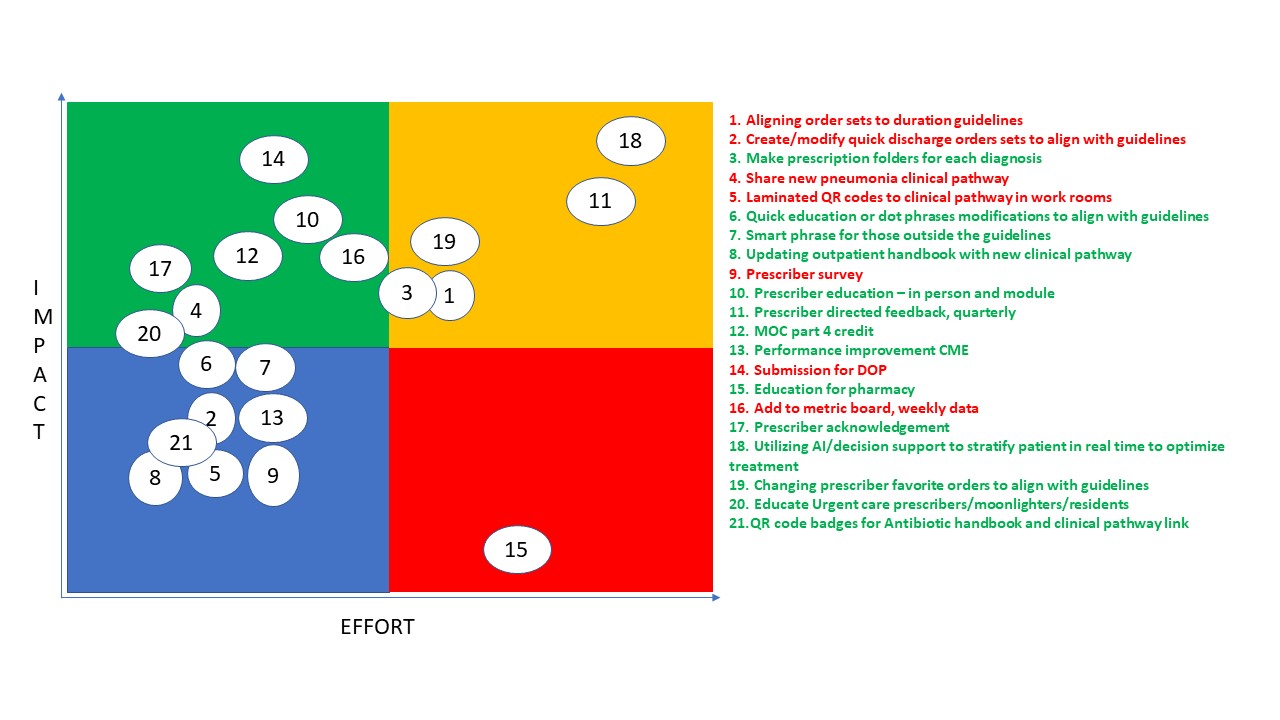 The numbered intervention items on the right correspond to the numbers plotted on the graph to the left. Intervention items highlighted in red have already been completed or are in the process of being completed, items highlighted in green indicate possible future interventions.
The numbered intervention items on the right correspond to the numbers plotted on the graph to the left. Intervention items highlighted in red have already been completed or are in the process of being completed, items highlighted in green indicate possible future interventions.Percentage of patients receiving suggested duration for CAP and ABRS, combined and individual p charts
.png) Annotated control charts showing the outcome metric: percentage of children prescribed the suggested duration for CAP and ABRS in the ED; total number (N) of patients included per month.
Annotated control charts showing the outcome metric: percentage of children prescribed the suggested duration for CAP and ABRS in the ED; total number (N) of patients included per month.Key Driver Diagram
Prioritization Matrix
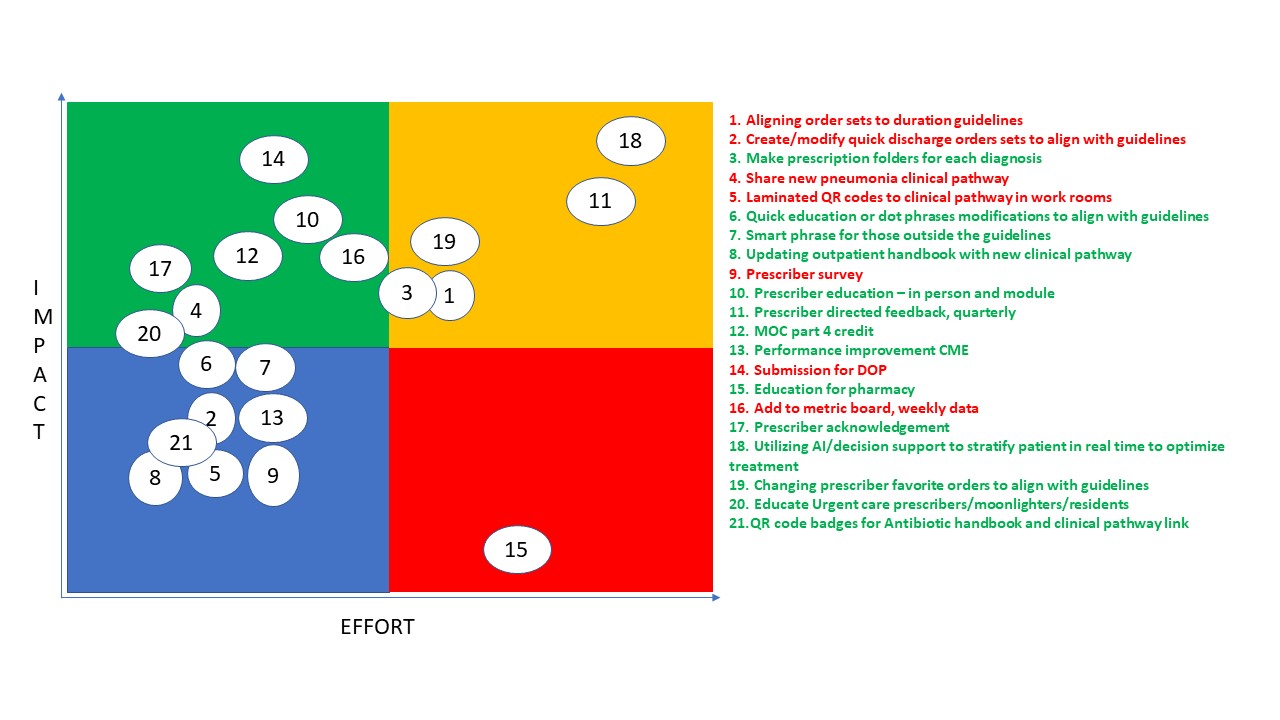 The numbered intervention items on the right correspond to the numbers plotted on the graph to the left. Intervention items highlighted in red have already been completed or are in the process of being completed, items highlighted in green indicate possible future interventions.
The numbered intervention items on the right correspond to the numbers plotted on the graph to the left. Intervention items highlighted in red have already been completed or are in the process of being completed, items highlighted in green indicate possible future interventions.Percentage of patients receiving suggested duration for CAP and ABRS, combined and individual p charts
.png) Annotated control charts showing the outcome metric: percentage of children prescribed the suggested duration for CAP and ABRS in the ED; total number (N) of patients included per month.
Annotated control charts showing the outcome metric: percentage of children prescribed the suggested duration for CAP and ABRS in the ED; total number (N) of patients included per month.

