Hospital Medicine 1: Quality Improvement
Session: Hospital Medicine 1: Quality Improvement
549 - Development and implementation of a bronchiolitis conditional discharge workflow: A pilot study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 549.4252
Michelle Noelck, Oregon Health and Science University, Portland, OR, United States; Alexandra M. Haigh, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States; Jaclyn JA. Bowker, Oregon Health & Science University School of Medicine, Portland, OR, United States; Michael J. Jones, Doernbecher Children's Hospital at Oregon Health & Science University, Lake Oswego, OR, United States

Michelle Noelck, MD (she/her/hers)
Professor of Pediatrics
Oregon Health and Science University
Portland, Oregon, United States
Presenting Author(s)
Background: Bronchiolitis is the leading cause of hospital admission in the first year of life, with increasing cost associated with care. Hospital admission is disruptive for patients and families, associated with missed work for caregivers, lost wages, and separation of the family unit.
Objective: Our global aim was to discharge healthy infants with bronchiolitis when medically ready. Our specific aim was to develop and implement a bronchiolitis conditional discharge workflow at a medium sized academic center with 50% of eligible patients having this order placed over the subsequent viral season.
Design/Methods: Stakeholders including nurse, physician and respiratory therapy leadership gathered to review current literature and define bronchiolitis discharge criteria. These criteria included: 1) room air saturation of >88% for >4 hours 2) mild bronchiolitis severity scores 3) ability to maintain hydration by mouth 4) no longer requiring mechanical suction and 5) caregivers comfortable with discharge. We conducted 3 PDSA cycles: 1) creation of a bronchiolitis conditional discharge order, which would allow the bedside nurse to discharge a patient once discharge criteria were met without re-examination by the medical team 2) discharge summary and after visit summary templates and 3) a progress note template that included a prompt for the conditional discharge workflow. Primary outcome measure was percentage of patients who had the bronchiolitis conditional discharge order placed. Process measure was the percentage of patients where new documentation tools were utilized. Balancing measures were length of stay (LOS) and 3-day readmission rate. Process and outcome measures were collected via monthly EMR reports and retrospective chart review, and tracked via run chart.
Results: Stakeholders created a key driver diagram to guide the work (Figure 1). During the implementation season, 80 eligible patients were identified; 54% had at least one of the newly created documentation tools utilized, and 38% had a bronchiolitis conditional discharge order placed (Figure 2). There was no change in LOS or 3-day readmission rate.
Conclusion(s): Bronchiolitis discharge criteria were identified by an interprofessional team and successfully implemented using a conditional discharge order. Following implementation of the new order, 38% of eligible patients were discharged using the conditional discharge criteria workflow. There was no change in hospital LOS or 3-day readmission rate. Continued improvement efforts and data collection are ongoing this bronchiolitis season.
Figure 1
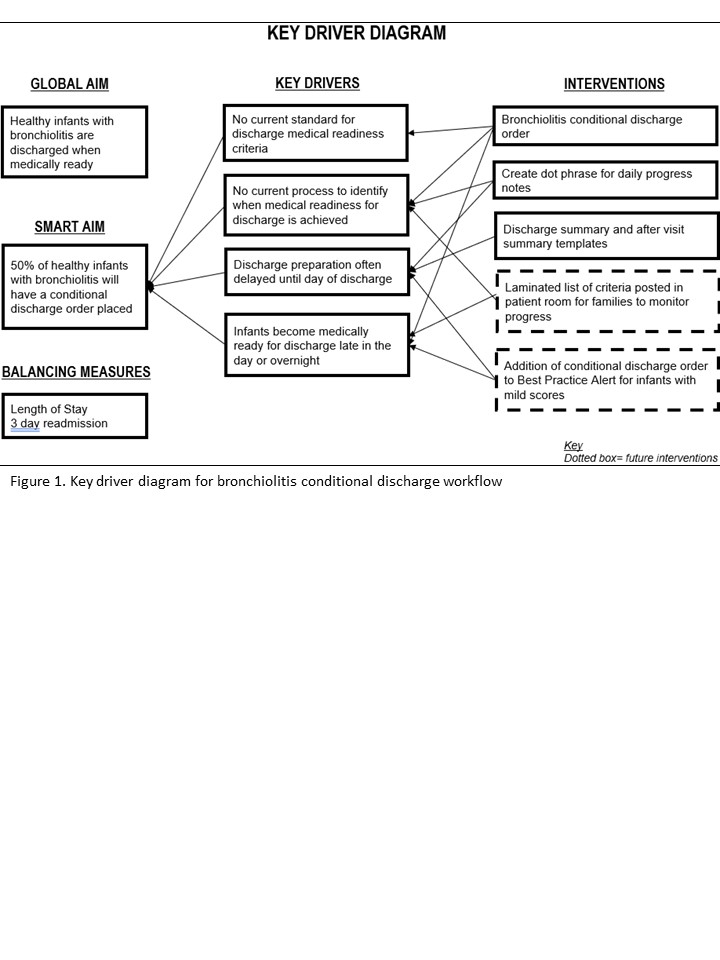 Key driver diagram for the bronchiolitis conditional discharge workflow
Key driver diagram for the bronchiolitis conditional discharge workflowFigure 2
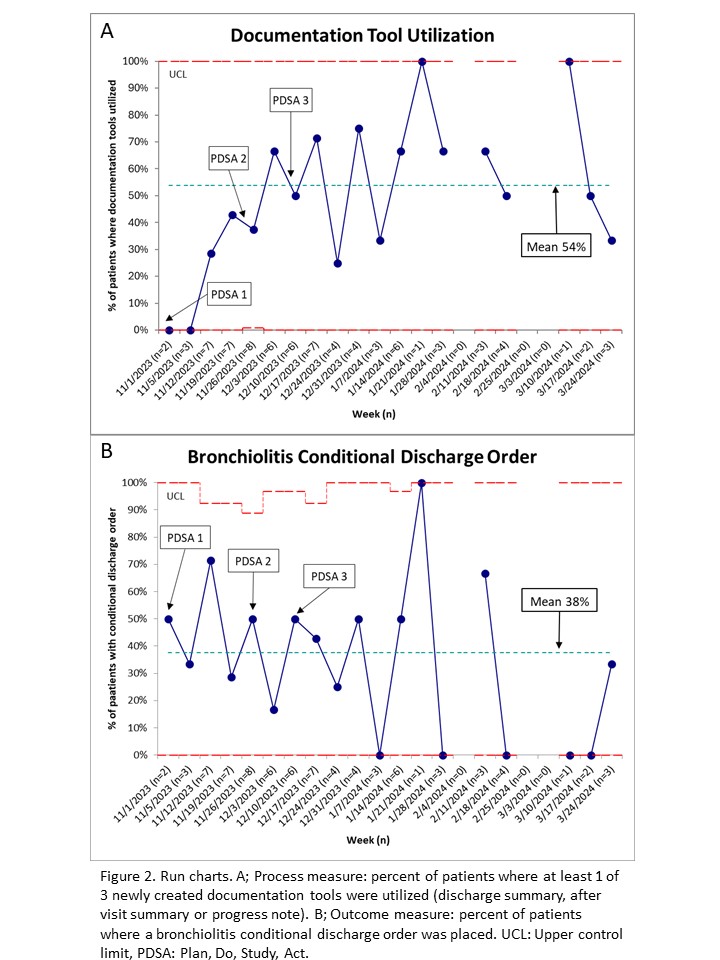 Run charts. A; Process measure: percent of patients where at least 1 of 3 newly created documentation tools were utilized (discharge summary, after visit summary or progress note). B; Outcome measure: percent of patients where a bronchiolitis conditional discharge order was placed. UCL: Upper control limit, PDSA: Plan, Do, Study, Act.
Run charts. A; Process measure: percent of patients where at least 1 of 3 newly created documentation tools were utilized (discharge summary, after visit summary or progress note). B; Outcome measure: percent of patients where a bronchiolitis conditional discharge order was placed. UCL: Upper control limit, PDSA: Plan, Do, Study, Act.

