Mental Health 2
Session: Mental Health 2
770 - COVID-19 Infection is Associated with Incident Prescription of Antidepressants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 770.4240
Cade M. Nylund, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Apryl Susi, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Zella Berill, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Elizabeth J. Hisle-Gorman, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States

Cade M. Nylund, MD
Professor of Pediatrics
Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine
Bethesda, Maryland, United States
Presenting Author(s)
Background: COVID-19 infection has been shown to increase clinical rating scores for anxiety and depression. It is not known whether COVID-19 infection is associated with the development of mental health symptoms requiring pharmaceutical treatment.
Objective: This study evaluates the causal relationship between COVID-19 infection and incident initiation of treatment with antidepressants.
Design/Methods: A propensity score-matched cohort study using the Military Health System Database data for children 0-17 years of age was performed. ICD-10 codes and laboratory tests identified patients with COVID-19 infections from July 2020 to June 2021. Counts of all inpatient and outpatient diagnoses, procedures, and outpatient medication prescription data one year preceding the COVID-19 infection were categorized according to clinical classification software. Using 1770 clinical variables, age, sex and month, a propensity score for COVID-19 exposure was matched 2:1 non-exposed to exposed and on age and sex. Dispensed antidepressants in the categories listed in Table 1 were aggregated. Any subject who had a prescription in the year before their cohort entry date were excluded. Participants were followed for a year with time to censoring as either loss to follow-up or infection with COVID-19. Cox Proportional Hazards Model was used.
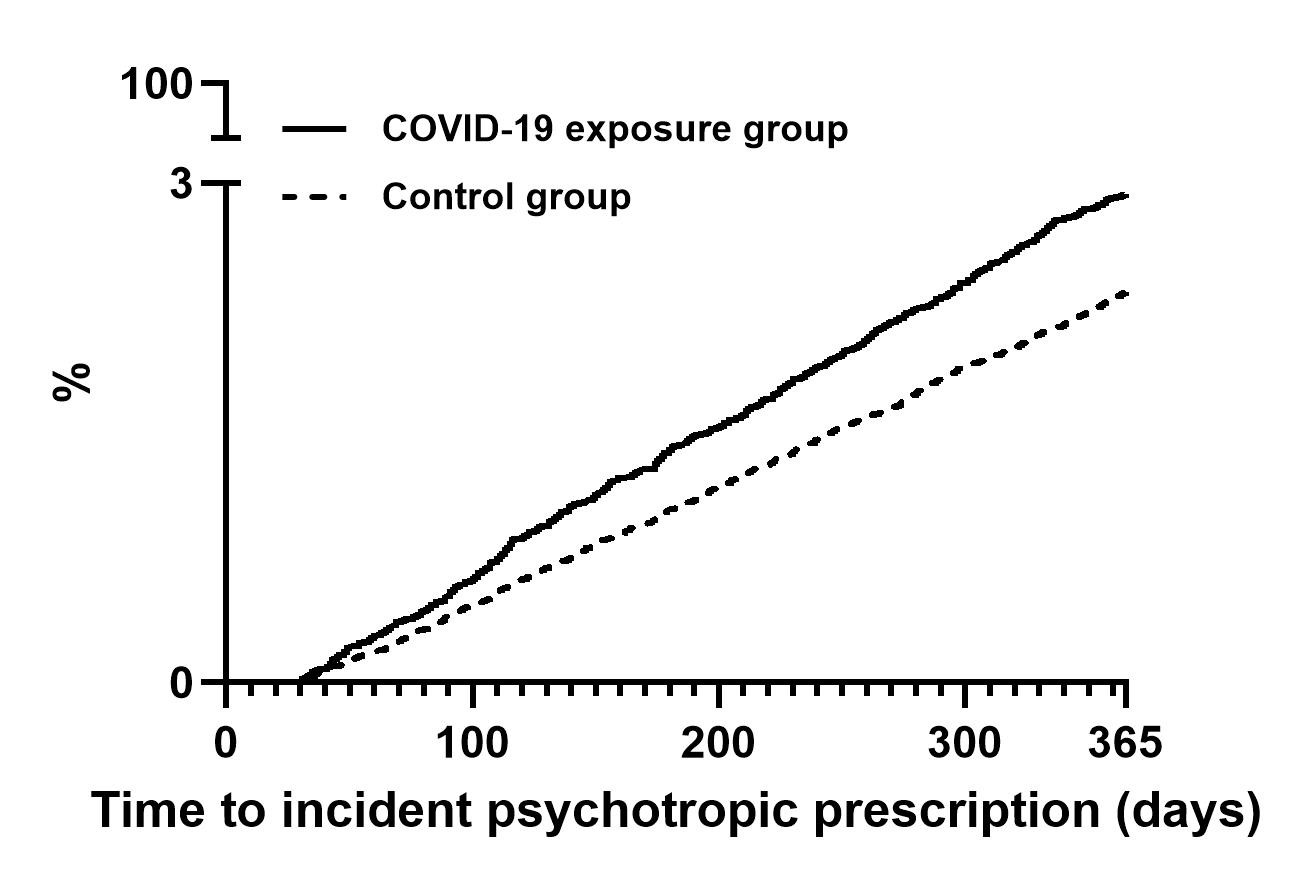
Results: There were 61,170 participants in the study, 20,390 with COVID-19 and 40,780 controls. 47.70% were female and median age was 10 (interquartile range [IQR], 5-14). 1,502 subjects were prescribed antidepressants for the first time; 590 (2.89%) with COVID-19 infection and 912 (2.24%) among controls. The number of new prescriptions in each class of antidepressants are listed in Table 1. The median age for those prescribed an antidepressant was 14 years; IQR, 12-16) and 66.1% were female (n= 993). Children with COVID-19 were more likely to have a new antidepressant prescribed (HR, 1.26; 95% confidence interval, 1.14- 1.40; see figure 1), however after adjusting for pre-COVID-19 counts of healthcare utilization the association of COVID-19 became insignificant (p=0.09).
Conclusion(s): Children 0-17 years of age diagnosed with COVID-19 had a higher risk of newly prescribed antidepressants. Statistical significance was lost after adjusting for prior healthcare utilization suggesting pre-existing conditions were effect modifiers and healthcare seeking behavior may have confounded results. Understanding how COVID-19 exacerbates and affects the development of mental health will assist in more effective screening, diagnosis and treatment strategies.
Table 1 Number of New Antidepressant Prescriptions by Medication Class in Cohort
Medication Class table.pdf
Figure 1 Cumulative Incidence Percent of Subjects with a Newly Prescribed Antidepressant by COVID-19 Exposure Status