Mental Health 2
Session: Mental Health 2
771 - Depression Trajectories Across Early Childhood for Mothers of Infants Born Very Preterm
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 771.4235
Alexandrea L.. Craft, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Marie Camerota, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Brian S.. Carter, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Jennifer Check, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Jennifer helderman, WFB1-AtriumWH, Clemmons, NC, United States; Julie Hofheimer, University of North Carolina at Chapel Hill, Durham, NC, United States; Elisabeth McGowan, Women & Infants Hospital of Rhode Island, Barrington, RI, United States; Charles R. Neal, University of Hawaii John A Burns School of Medicine, Kailua, HI, United States; Thomas MD. O'Shea, UNC Chapel Hill, Chapel Hill, NC, United States; Steven L. Pastyrnak, Michigan State University College of Human Medicine, Grand Rapids, MI, United States; Lynne Smith, Harbor UCLA Medical Center, Torrance, CA, United States; Lynne M. Dansereau, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Sheri A. DellaGrotta, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Carmen J. Marsit, Emory University Rollins School of Public Health, Atlanta, GA, United States; Barry Lester, The Warren Alpert Medical School of Brown University, Providence, RI, United States

Alexandrea L. Craft, PhD (she/her/hers)
Assistant Professor
The Warren Alpert Medical School of Brown University
Providence, Rhode Island, United States
Presenting Author(s)
Background: Postpartum depression or severe psychological distress has been reported by 18-43% of mothers with preterm infants. Prior research examined depression trajectories in mothers of preterm infants using very broad definitions of prematurity (> 22 weeks - < 37 weeks gestation). The influence of infants’ illness acuity and chronicity experienced by mothers of very preterm infants (VPI; < 30 weeks’ gestation) who are at increased risk for depression or recurring psychological distress is not known.
Objective: Describe depression risk over time by characterizing depression trajectories in a high-risk sample of mothers of VPI.
Design/Methods: Neonatal Neurobehavior and Outcomes in Very Preterm Infants Study followed 584 VPI from 9 US university NICUs. Mothers reported depressive symptoms using the Brief Symptom Inventory (BSI), depression subscale, at NICU discharge and 2, 3, and 5 years of age. T scores ≥ 63= clinically significant distress; > 50=at risk. We applied growth mixture modeling (GMMs) to identify subgroups of mothers with different depression trajectories. Multinominal logistic regressions tested associations among trajectory groups and sample characteristics.
Results: A Latent growth curve model confirmed that a linear trajectory fit the data well (CFI = .97, TLI = .95, RMSEA = .03). We then estimated GMMs with 1–5 trajectory profiles. Based on fit statistics (Table 1), we determined that a 4-profile solution best fit the data. We compared maternal and infant characteristics by profile (Table 2). Mothers in profile 1 (4%, n=22) showed clinically significant depressive symptoms at NICU discharge which decreased over time and became non-clinical by age 5 (Figure 1). Their infants were more likely to have longer NICU stays compared to infants of mothers in the low, stable group (Profile 3; OR = 1.01, 95%CI 1.00-1.02). Profile 2 mothers (13%, n=78) showed depressive symptoms in the At-Risk range which decreased over time. Finally, profile 3 mothers (64%, n=373) showed non-clinical depressive symptoms that increased over time while profile 4 mothers (19%, n=111) showed stable non-clinical depressive symptoms over time.
Conclusion(s): This is one of the first studies to look at depression trajectories in mothers of VPI. Results showed elevated depression symptoms were associated with lengthier NICU stays, and varied decrements among trajectories over time. Findings suggest continued need for screening to prevent persisting depression symptoms across early childhood, especially for mothers of VPI who demonstrate needs for more support and developmental follow-up.
Figure 1. Latent Class Depression Profiles - Four Profile Solution
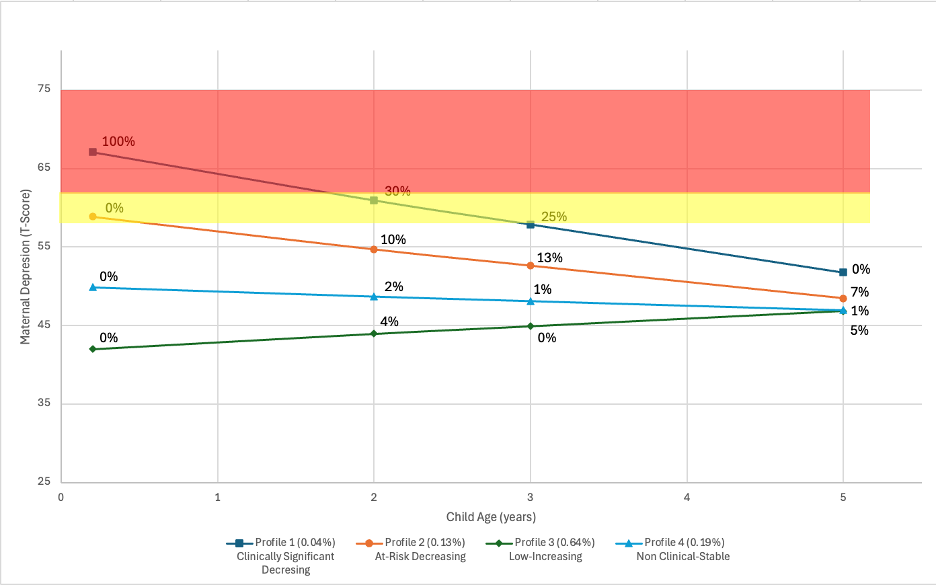 Note: percentage in figure indicates percent of the group that is in the clinically significant range for depressive symptoms (T-score ≥ 63).
Note: percentage in figure indicates percent of the group that is in the clinically significant range for depressive symptoms (T-score ≥ 63).Table 1. Growth Mixture Model Fit Statistics
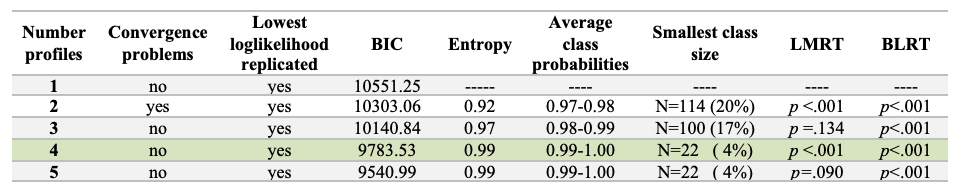 Note: Four class solution was chosen because while it included a small class, it still had a significant LMRT and good entropy and BIC values.
Note: Four class solution was chosen because while it included a small class, it still had a significant LMRT and good entropy and BIC values. Table 2. Sample Characteristics by Latent Class Depression Profile
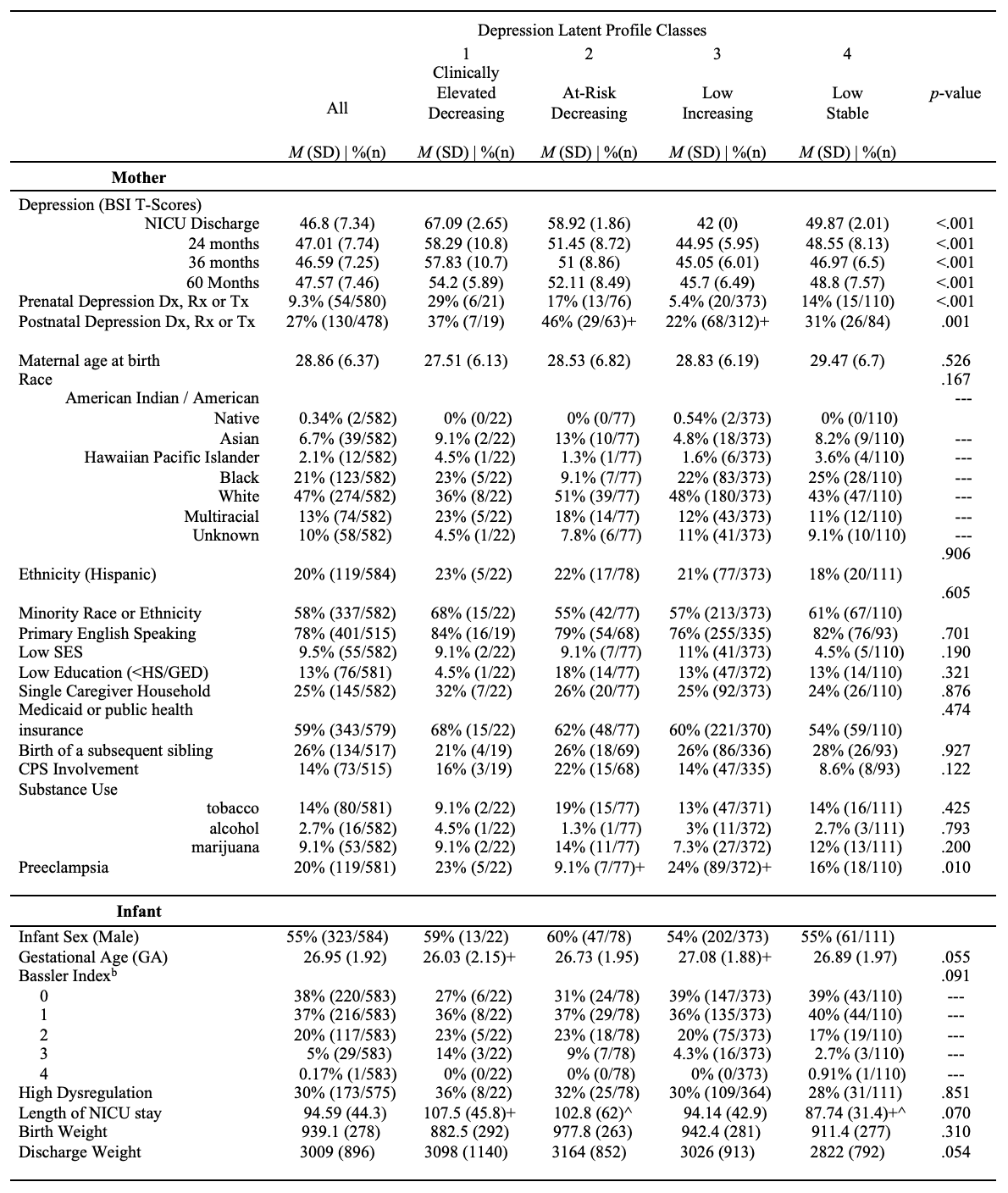 Note: Sample size is 584 mothers. a Minority racial or ethnic group included American Indian, Asian, Black, Hispanic, Native Hawaiian, Pacific Islander, or “other,”. b Bassler index is a cumulative neonatal morbidity risk score that includes severe retinopathy of prematurity (ROP), bronchopulmonary dysplasia (BPD), brain injury (parenchymal echodensity, periventricular leukomalacia and ventricular dilation), necrotizing enterocolitis (NEC) and sepsis; higher numbers represent greater risk. p-values correspond to multinomial logistic regression test statistics. +/^ indicates significant group difference (p < .05)
Note: Sample size is 584 mothers. a Minority racial or ethnic group included American Indian, Asian, Black, Hispanic, Native Hawaiian, Pacific Islander, or “other,”. b Bassler index is a cumulative neonatal morbidity risk score that includes severe retinopathy of prematurity (ROP), bronchopulmonary dysplasia (BPD), brain injury (parenchymal echodensity, periventricular leukomalacia and ventricular dilation), necrotizing enterocolitis (NEC) and sepsis; higher numbers represent greater risk. p-values correspond to multinomial logistic regression test statistics. +/^ indicates significant group difference (p < .05)
