Technology 2: Telemedicine
Session: Technology 2: Telemedicine
188 - Feasibility of Using Low-Cost Mobile Video Technology to Assess Respiratory Effort in Children in Moving Ambulances
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 188.4792
Ryan Brewster, Ariadne Labs, Brigham and Women's Hospital, Boston, MA, United States; Monica E.. Kleinman, Boston Children's Hospital, Boston, MA, United States; Pamela Hall, Boston Children's Hospital, Boston, MA, United States; Michael O'Melia, Boston Children's Hospital Critical Care Transport Team, Stoneham, MA, United States; Jamie R. Moore, Boston Children’s Hospital, South Easton, MA, United States; Jordan Sage. Rettig, Boston Children's Hospital, Boston, MA, United States; Ashley Gorman, Boston Children’s Hospital, Norwood, MA, United States; Ijeoma M. Okafor, Boston Medical Center, Boston, MA, United States; Howard J.. Cabral, Boston University School of Public Health, Boston, MA, United States; Carlos A. Camargo, MGH / Harvard University, Boston, MA, United States; James Feldman, Boston University School of Medicine, Boston, MA, United States; Tehnaz Boyle, Boston Medical Center, Boston, MA, United States

Ryan Brewster, MD
Resident Physician
Ariadne Labs, Brigham and Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Despite national guidance to integrate digital technology in prehospital care, few Emergency Medical Service (EMS) systems use video for telehealth. Pediatric respiratory illness is a common reason for EMS transport. Whether off-the-shelf mobile technology can be used to assess respiratory effort in a child secured for transportation in a moving ambulance is unknown.
Objective: To test the feasibility of using low-cost mobile technology to assess respiratory effort in children in moving ambulances
Design/Methods: This is an open-label, non-randomized pilot feasibility trial (NCT05967624) of children transported by a pediatric critical care transport team in Massachusetts (June-December 2024) using Zoom Pro, HIPAA-compliant video software, on tablet devices. We included children aged < 18 years transported for acute respiratory illness. We excluded children with non-respiratory complaints, non-English speaking parents/guardians, those needing resuscitation procedures for life-threatening illness in the ambulance, and minor wards of the state. After consent, transport nurses (n=3) initiated a video-call from the moving ambulance to remote physicians on-call (n=2). The transport nurse observed the child in the ambulance to score the Respiratory Observation Checklist (9 physical signs, 1 global measure of respiratory distress). The remote physician observed the child via streaming video to score the checklist independently. We measured feasibility (primary outcome) as interrater agreement in global assessment of respiratory distress; and usability, call success rate, and potential adverse events (secondary outcomes) on post-call questionnaires. We report descriptive statistics and percent agreement (scale: 0.01-0.20=poor, 0.21-0.40=fair, 0.41-0.60=moderate, 0.61-0.80=good, and 0.81-1.0=excellent) as preliminary analysis as enrollment is ongoing.
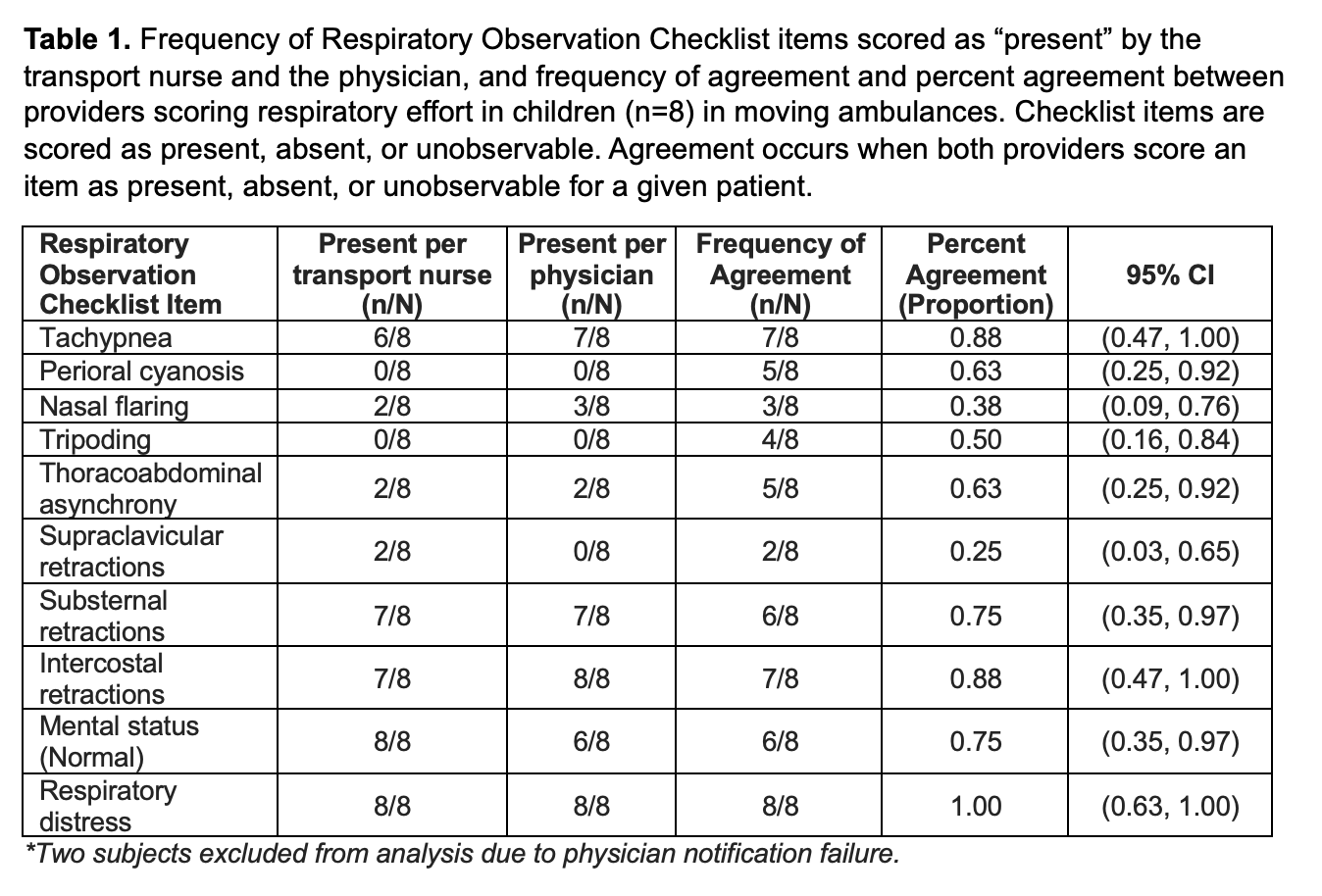
Results: We enrolled 10 (50%) of planned 20 children (median age=2.9 years; IQR 0.1-5.0). We found 100% agreement [95% CI 0.63, 1.00] in global assessment of respiratory distress between providers (Table 1). The mean total usability score was 5.2 (SD=0.6) of a maximum 7. Three (30%) calls connected in ≤2 attempts, 5 (50%) in ≥3 attempts, and 2 (20%) did not connect. Inconsistent physician alerts and cybersecurity protections hindered connection success. There were no adverse events.
Conclusion(s): Assessing a child’s respiratory effort using low-cost mobile technology is feasible in a moving ambulance. Using standardized dispatch mechanisms to alert physicians could enhance reliability and efficiency of connections.
Frequency of Respiratory Observation Checklist items scored as “present” by the transport nurse and the physician, and frequency of agreement and percent agreement between providers scoring respiratory effort in children (n=8) in moving ambulances. Checklist items are scored as present, absent, or unobservable. Agreement occurs when both providers score an item as present, absent, or unobservable for a given patient