Hematology/Oncology 2: Pediatric Hematology
Session: Hematology/Oncology 2: Pediatric Hematology
111 - Evaluating Emergency Department Referrals and Pediatric Provider “Comfort” in managing Iron Deficiency Anemia in Pediatric Patients
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 111.4755
Allysen Dubisky, University of Texas at Austin Dell Medical School, Austin, TX, United States; Matthew Wilkinson, University of Texas at Austin Dell Medical School, Austin, TX, United States; Ginna Priola, Dell Children's Medical Center of Central Texas, Austin, TX, United States

Allysen Dubisky, MD (she/her/hers)
Resident
University of Texas at Austin Dell Medical School
Austin, Texas, United States
Presenting Author(s)
Background: Iron deficiency anemia (IDA) is the most common nutritional disorder in the world. The American Academy of Pediatrics provides specific recommendations on screening, diagnosis, and management of this disease. Studies have shown that patients receive inappropriate oral iron doses, are frequently referred to the emergency department (ED) by their primary care physician for evaluation of anemia that could have been managed outpatient, and are increasingly requiring hospital admissions for potential blood transfusions.
Objective: To evaluate local pediatrician comfort in managing iron deficiency anemia in the outpatient setting. To identify the number of unnecessary ED referrals by primary care providers for iron deficiency anemia in pediatric patients.
Design/Methods: This study is a retrospective chart review of pediatric patients aged 0-18 years old who were referred, evaluated, and treated for iron deficiency anemia between July 1, 2022 through September 31, 2024 at a large, freestanding, urban, tertiary pediatric hospital and satellite hospital. We collected data on patient demographics as well as laboratory and management data during their hospital stay. Three physicians reviewed each chart to determine the necessity of the ED referral based on emergent treatment or hospital admission. We also provided electronic surveys to community pediatricians to evaluate their level of comfortability in managing iron deficiency anemia in the clinic.
Results: Forty-six pediatric patients were identified for our study. Forty-two patients (91.3%) were able to be discharged home without any emergent intervention (95% CI: 79.2 to 97.6). One patient (2.2%) received a blood transfusion in the ED and was then discharged home on oral iron. One patient (2.2%) required admission to the pediatric intensive care unit and two patients (4.3%) required admission to the inpatient service.
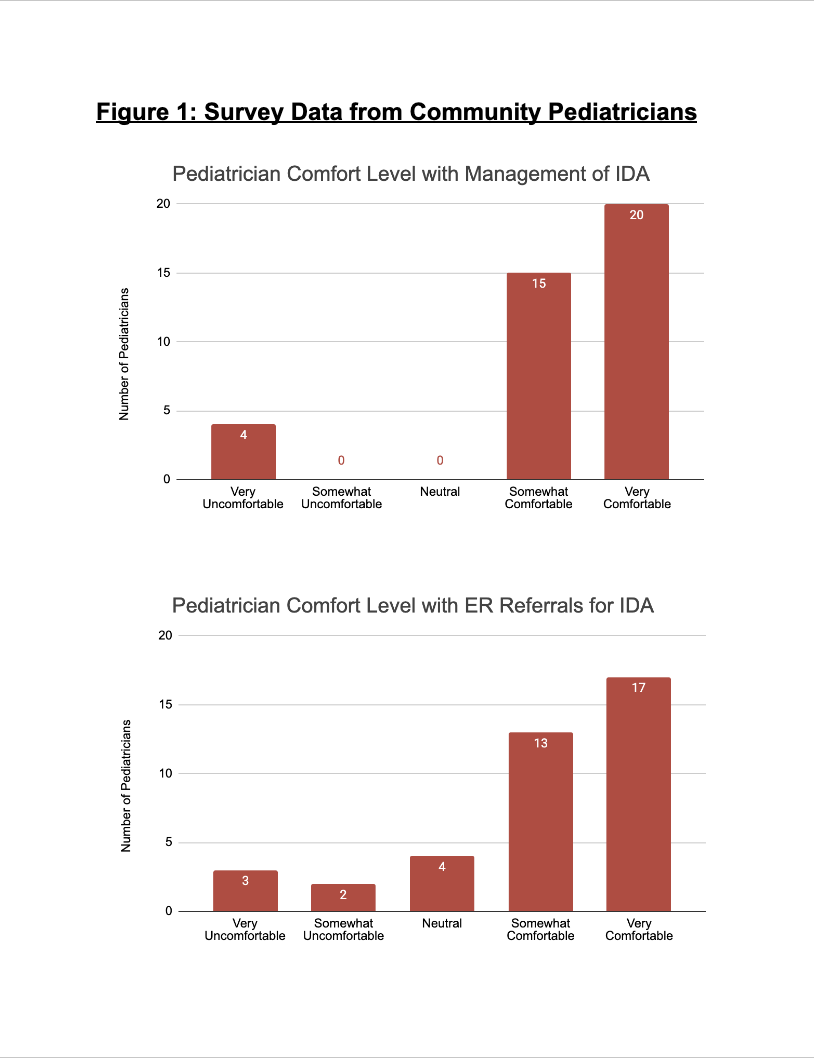
Thirty-nine community pediatricians participated in our survey. While many (90%) reported they are comfortable with diagnosing and managing IDA, 23% reported being neutral to very uncomfortable knowing when to refer to a hematologist or to the ED. Patient compliance was the most commonly reported barrier (77%) to providing appropriate care.
Conclusion(s): While many pediatricians in our study reported comfortability with IDA diagnosis and management, there continue to be many unnecessary ED referrals with very few patients requiring transfusions or hospitalization. Further investigation is required to better understand this discrepancy of improper allocation of resources, including ED referrals, hospitalizations, and blood transfusions.
Table 1: Demographic Characteristics
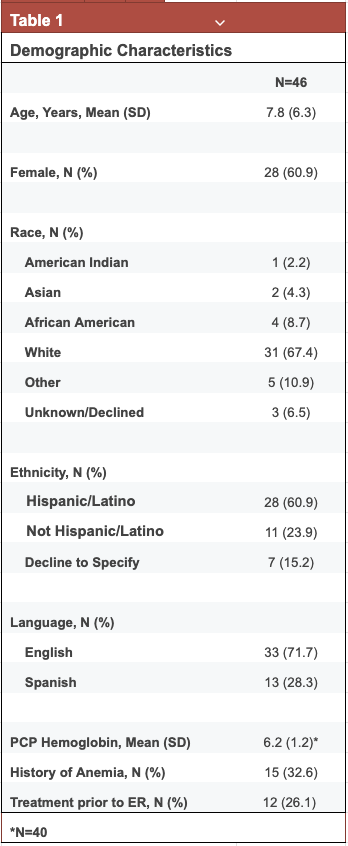
Table 2: Hospital Labs and Outcomes
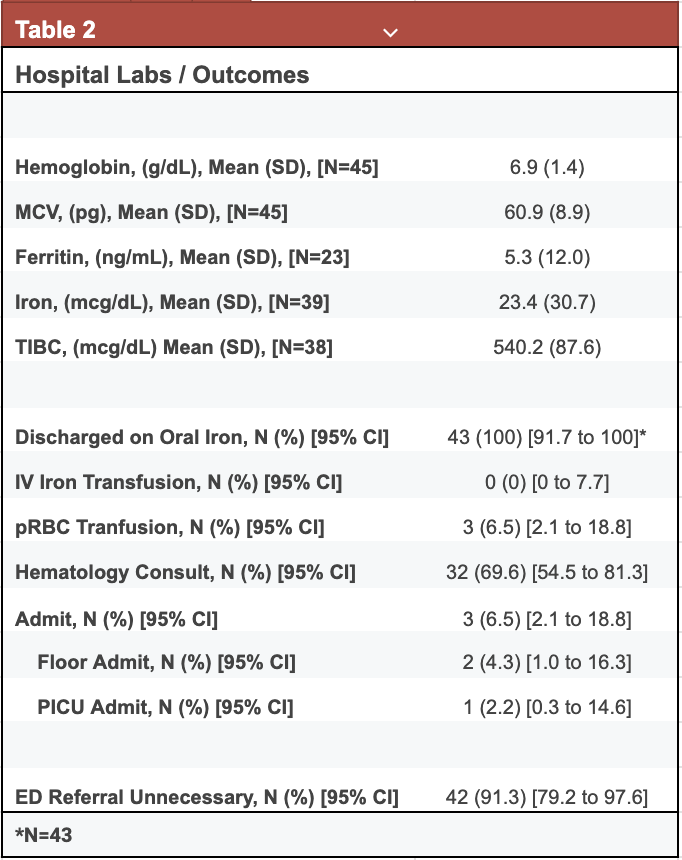
Figure 1: Survey Data from Community Pediatricians