Neonatal Nephrology/AKI 2
Session: Neonatal Nephrology/AKI 2
019 - Epidemiology and Outcome of Acute Kidney Injury in a Quaternary Referral Neonatal Intensive Care Unit
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 19.4831
Thomas A. Forbes, Murdoch Children's Research Institute, Melbourne, Victoria, Australia; Peter R. Summers, Murdoch Children's Research Institute, Parkville, Victoria, Australia; Alice Voskoboynik, The Royal Children's Hospital, Melbourne, Victoria, Australia; Simon Carter, The Royal Children's Hospital Melbourne, Parkville, Victoria, Australia; Ruth K. Armstrong, The Royal Children's Hospital, Melbourne, Victoria, Australia; Emily See, Royal Melbourne Hospital, Melbourne, Victoria, Australia

Thomas A. Forbes, MBBS FRACP PhD (he/him/his)
Paediatric Nephrologist
Murdoch Children's Research Institute
Melbourne, Victoria, Australia
Presenting Author(s)
Background: Acute kidney injury (AKI) in the neonatal intensive care unit (NICU) occurs in up to 35% of neonates and is associated with mortality.
Objective: We aimed to describe the epidemiology and outcomes of AKI in a quaternary referral (no inborn admissions), predominantly surgical, non-cardiac NICU.
Design/Methods: We extracted retrospective electronic medical record (EMR) data for all of neonates admitted to the Royal Children’s Hospital NICU, Melbourne, Australia between 1st January 2017 and 30th June 2023. Inclusion criteria were ≤28 days old on admission, admitted for ≥24 hours and at least 2 serum creatinine assays performed. Only the first admission for each infant was included. AKI was described by stage, frequency and duration using the Kidney Disease Improving Global Outcomes neonatal AKI (creatinine-based) definition. The primary outcome was 30-day mortality and secondary outcomes included major adverse kidney events at 30 days (MAKE30), length of NICU stay, AKI documentation, nephrology inpatient consultation and follow-up post-discharge.
Results: Among 2,024 admissions to the NICU during the study period, the median gestational age was 37+6 weeks (IQR 35+3 to 39+1) and the mean birth weight was 2.84kg (SD 0.87kg). Surgery was performed in 37.6% of the cohort. nAKI occurred in 10.2% of infants (206/2024; 253 episodes; 5.4 episodes per 1000 patient-days). Among infants suffering AKI, transient and persistent stage 1 AKI were most common (17% and 22% respectively). AKI was associated with an increased risk of 30-day mortality (aOR 4.2; 95%CI 2.4-7.2). Neonates with AKI were more likely to develop a MAKE30 (aOR 11.6; 95%CI 7.1-18.9). There was a progressive increase in risk of mortality and MAKE30 with increasing AKI stage but correlation with AKI duration or recurrence was less clear. The median length of NICU stay was longer in the AKI cohort (median days [IQR]: 49[18-114] vs 11[5-29]; z = -12.8; p< 0.0001). Within the AKI cohort, 20% had the AKI documented in the diagnosis list, 24% were consulted by nephrology in hospital, and 22% of neonates discharged locally (15/69) were followed up in the nephrology clinic.
Conclusion(s): Neonatal AKI is less frequent in our quaternary NICU compared to previous reports, potentially due to the higher gestational age and birth weight in the quaternary referral context. However, the association of AKI with mortality and increased length of NICU stay are similar to existing literature. This automated, data-driven approach could be adapted to monitor AKI rates in real time and to assess implementation of AKI quality improvement projects.
Figure 1
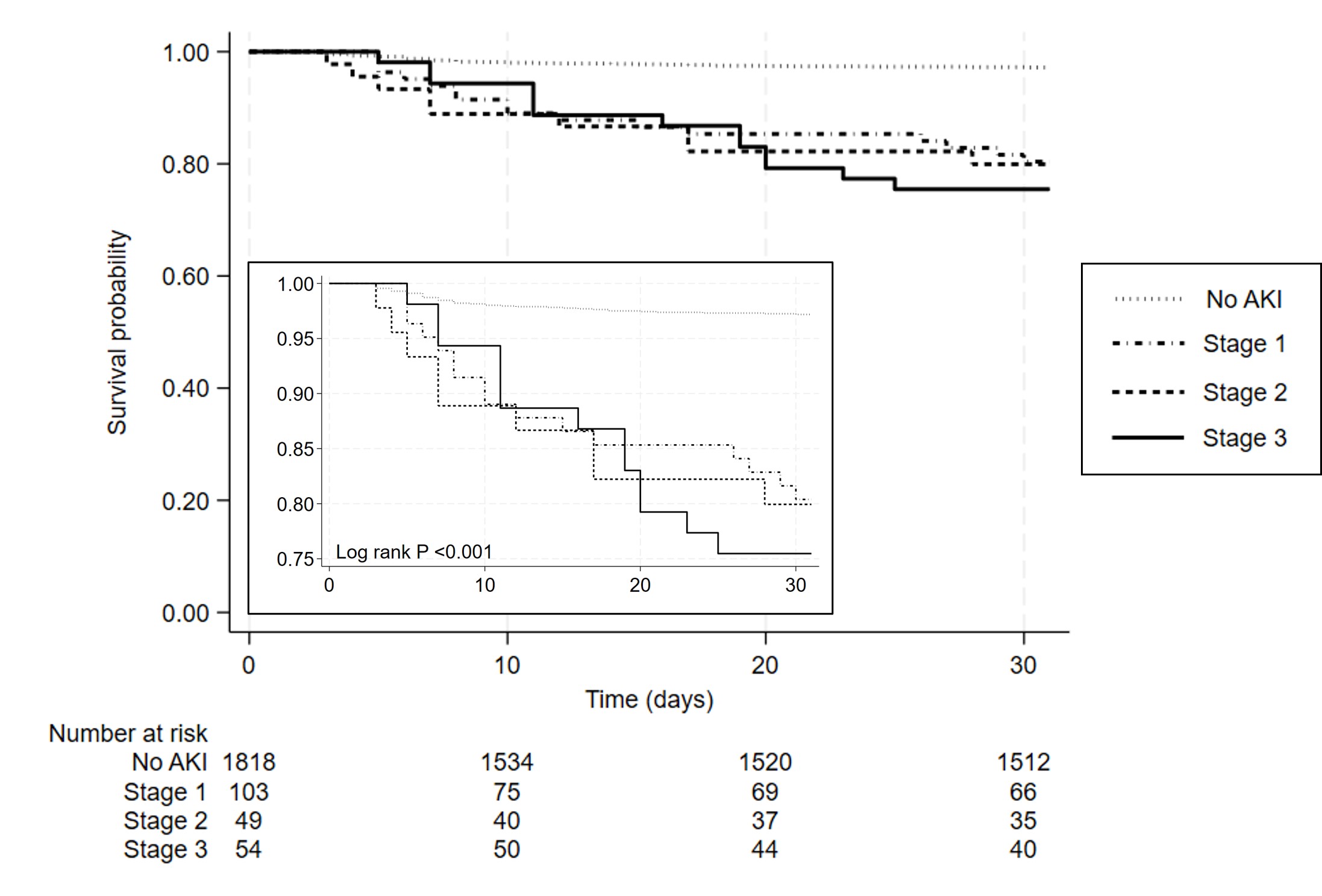 Survival curve for 30 day mortality in 2024 neonates admitted to a quaternary referral NICU according to AKI Stage by modified neonatal KDIGO (creatinine-based only) definition.
Survival curve for 30 day mortality in 2024 neonates admitted to a quaternary referral NICU according to AKI Stage by modified neonatal KDIGO (creatinine-based only) definition. 
