Emergency Medicine 6
Session: Emergency Medicine 6
275 - Decreasing time to antibiotics in febrile oncology patients with central line in the pediatric emergency department; A Quality Improvement initiative
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 275.4124
Abbigayle K. Carlson, Children's Mercy Hospitals and Clinics, Overland Park, KS, United States; Stephanie Clark, Children's Mercy Hospitals and Clinics, Shawnee, KS, United States; Joel Thompson, University of Missouri-Kansas City School of Medicine, Kansas City, MO, United States; Christopher Kaberline, Children's Mercy Hospitals and Clinics, Prairie Village, KS, United States; Leslie Ann. Hueschen, Children's Mercy Hospital/ University of Missouri-Kansas City, Kansas City, MO, United States

Abbigayle K. Carlson, DO (she/her/hers)
Resident
Children's Mercy Hospitals and Clinics
Overland Park, Kansas, United States
Presenting Author(s)
Background: Oncology patients are at a high risk for sepsis, due to immunosuppression from chemotherapy and the presence of a central line. Due to the high risk of sepsis, these patients require antibiotics within 60 minutes of Emergency Department (ED) arrival as recommended by the Surviving Sepsis campaign. From Sept 2022-May 2023 we achieved this 38% of the time at Children’s Mercy ED.
Objective: By April 30th, 2024, we will increase the percentage of ED febrile oncology patients receiving antibiotics < 60 minutes of arrival from 36.6% to 80%, stratifying by race and ethnicity, to monitor for inequities.
Design/Methods: Our outcome measures were the percentage of ED febrile oncology patients with antibiotics given < 60 minutes of arrival and median time to antibiotic administration. Our process measures were percentage of standard order-set usage and percentage of patients with critical information notes. Our balance measure was time from arrival to ED triage. We created a process map and fishbone diagram to identify delays in antibiotic administration. We performed interventions with Plan-Do-Study-Act methodology. We implemented standing nursing orders to decrease time spent waiting for providers to order antibiotics (June 2024). Outpatient oncology providers created a Critical Information Note, directing prompt antibiotic administration prior to labs or consultation (August 2024). We engaged physicians and made this a Maintenance of Certification (MOC) project with monthly review of run charts (Oct 2024). We prioritized timely access of the patients’ central line with a nursing script used with families to explain the need to access their child’s central line quickly (Oct 2024) and created a Central Line Note, identifying the type of central line and needle size required for access (March 2024).
Results: With these interventions, antibiotic administration < 60 minutes of ED arrival in febrile oncology patients increased from 36.6% to 54%. Median time to antibiotics decreased from 71.5 minutes to 55 minutes (Figure 1, 2). Decrease in inequities were most significant in the Hispanic population (101 min to 77 min) (Figure 3). Total order set usage (0 to 83%) and critical information note placement increased (from 0 to 78%) in August 2023, without a shift in our balance measure.
Conclusion(s): We did not achieve our goal, but we improved the variability and percentage of febrile oncology patients receiving antibiotics < 60 minutes and saw decreases in inequities. The most impactful intervention was having nurses order antibiotics. Sustainability was achieved by providing MOC physician credit with monthly data review.
Figure 1
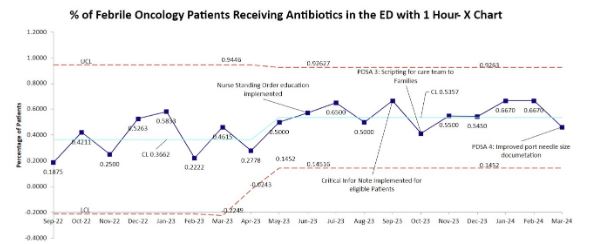 Percentage of ED febrile oncology patients with antibiotics < 60 min
Percentage of ED febrile oncology patients with antibiotics < 60 min Figure 2
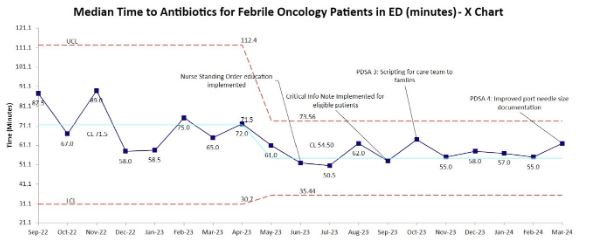 Median time to antibiotics in febrile oncology ED patients.
Median time to antibiotics in febrile oncology ED patients. Figure 3
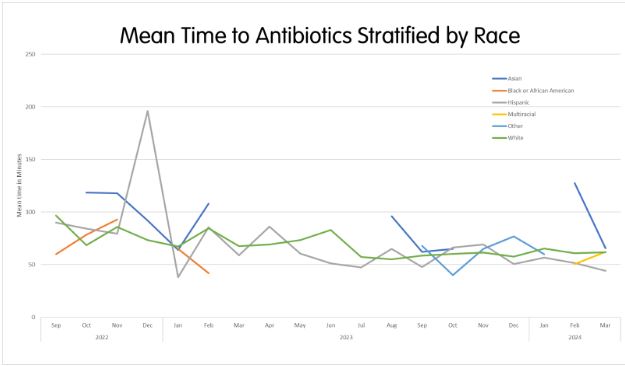 Time to antibiotics stratified by race/ethnicity
Time to antibiotics stratified by race/ethnicityFigure 1
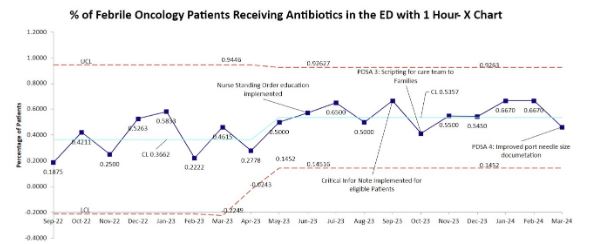 Percentage of ED febrile oncology patients with antibiotics < 60 min
Percentage of ED febrile oncology patients with antibiotics < 60 min Figure 2
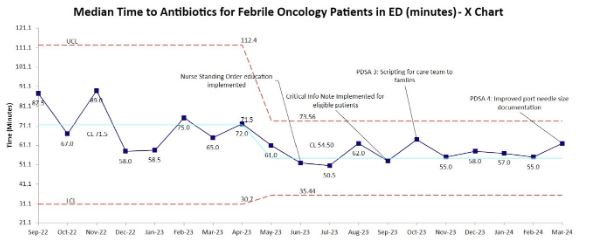 Median time to antibiotics in febrile oncology ED patients.
Median time to antibiotics in febrile oncology ED patients. Figure 3
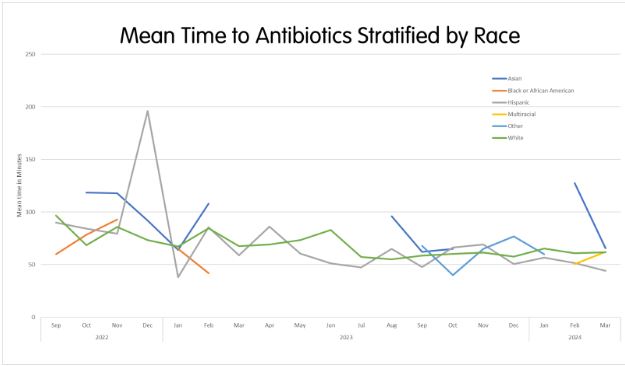 Time to antibiotics stratified by race/ethnicity
Time to antibiotics stratified by race/ethnicity

