Neonatal Hemodynamics and Cardiovascular Medicine 4
Session: Neonatal Hemodynamics and Cardiovascular Medicine 4
081 - Comparison of Heparin vs Bivalirudin With and Without Therapeutic Hypothermia in a Neonatal Porcine Model
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 81.4116
Laura A. Borruso, Uniformed Services University of the Health Sciences, Waipio, HI, United States; Lee-Ann Murata, Tripler Army Medical Center, Honolulu, HI, United States; Lauren Wong, Tripler Army Medical Center, Honolulu, HI, United States; Claudia A. Hernandez, Tripler Army Medical Hospital, Tripler AMC, HI, United States; Emily Bailey, Tripler, Honolulu, HI, United States; Lisa Pierce, Tripler Army Medical Center, Honolulu, HI, United States; Catherine Uyehara, Tripler Army Medical Center, Tripler AMC, HI, United States
- LB
Laura A. Borruso, MD (she/her/hers)
Neonatologist
Tripler Army Medical Center
Waipio, Hawaii, United States
Presenting Author(s)
Background: Therapeutic hypothermia is the standard of care treatment for neonates with moderate to severe hypoxic ischemic encephalopathy (HIE). HIE can be accompanied by cardiopulmonary dysfunction that requires the use of extracorporeal membrane oxygenation (ECMO) and administration of anticoagulants to reduce clot formation and thrombosis. It is unclear whether infants with HIE undergoing therapeutic hypothermia may have increased risk for intracranial bleeding due to anticoagulant use.
Objective: We hypothesized that hypothermia affects cerebral perfusion differently with anticoagulation. We tested whether the type of anticoagulant used would impact cerebral perfusion or bleeding differently by comparing the effects of heparin versus bivalirudin.
Design/Methods: Thirty-three anesthetized, mechanically ventilated Yorkshire-cross perinatal pigs were studied with core blood temperature at 38.4 + 0.1 o C (warm) or 34.5 + 0.1 o C (cold). Goal temperatures were achieved with ice packs and Bair Hugger. After baseline hemodynamics and blood gases were assessed, pigs were administered bivalirudin (0.2 mg/kg i.v.) or heparin (100 U/kg i.v.) followed by anticoagulant titration to achieve target activated clotting time (ACT, 162 + 3 seconds). Brain and systemic oxygen utilization, regional blood flow, and blood chemistries were assessed under 4 conditions: 1) no anticoagulation, warm; 2) no anticoagulation cold, 3) anticoagulation warm, 4) anticoagulation cold.
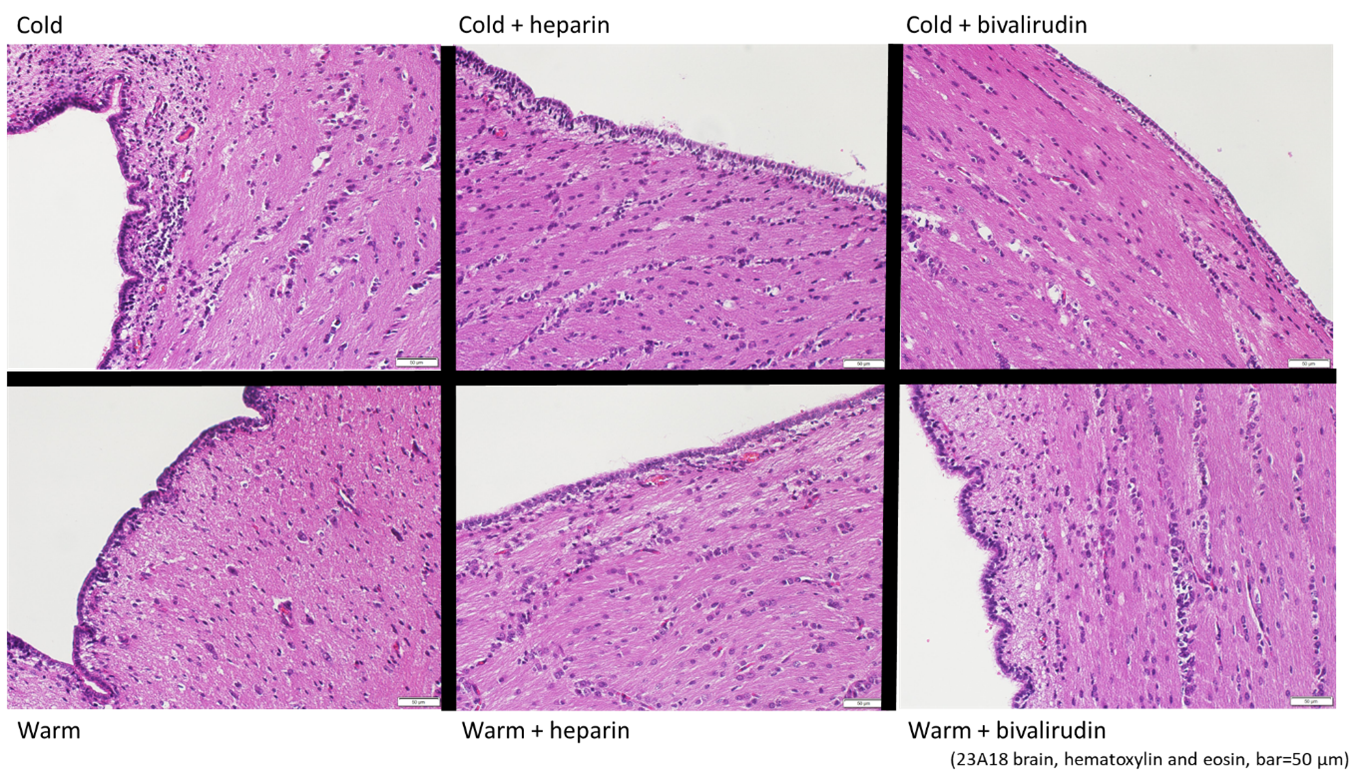
Results: Hypothermia decreased oxygen utilization with VO2 remaining constant in warm group but decreasing (p<0.05) from 5.8 + 0.5 ml/kg/min at baseline to 4.2 + 0.27 ml/kg/min after hypothermia. Hemoglobin levels were higher with cold 8.4 + 0.2 g/dL compared to warm 7.6 + 0.2 g/dL. Brain blood flow tended to decrease with the cold (fig 1). There was no differential response in the different brain regions. Anticoagulant treatment did not further affect the effect of temperature alone. There was no difference between the effects of heparin or bivalirudin. Histological assessment of brain regions (fig 2) indicate no apparent differences between temperature or anticoagulation treatments.
Conclusion(s): Results support the main effect of hypothermia causing a decrease in metabolism as evidenced by a drop in VO2 and fluid shifts as indicated by increased hemoglobin levels with cold. Anticoagulation treatment did not alter the changes caused by hypothermia. At the level and duration of anticoagulation achieved, there was no evidence of increased brain bleeding nor differences between heparin and bivalirudin.
Brain blood flow
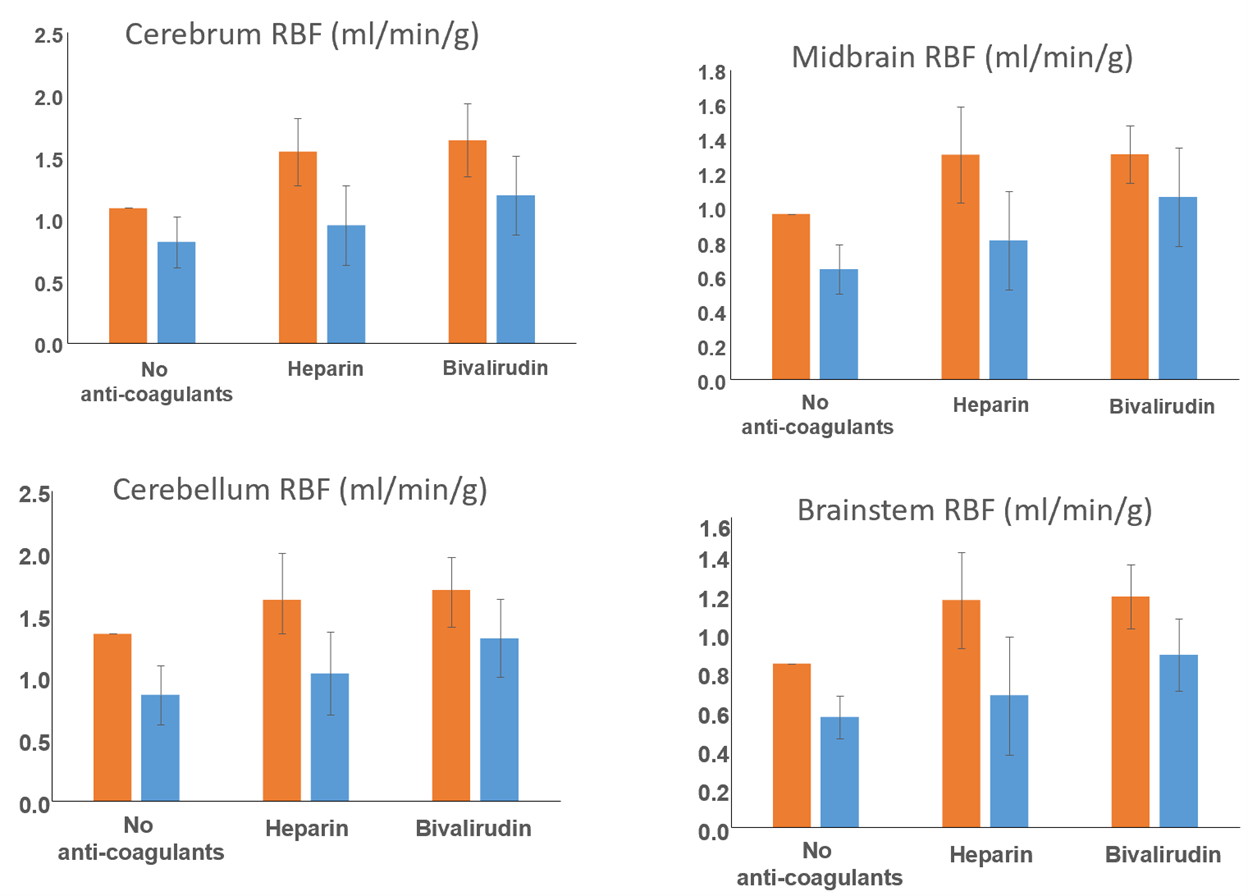
Representative histology images
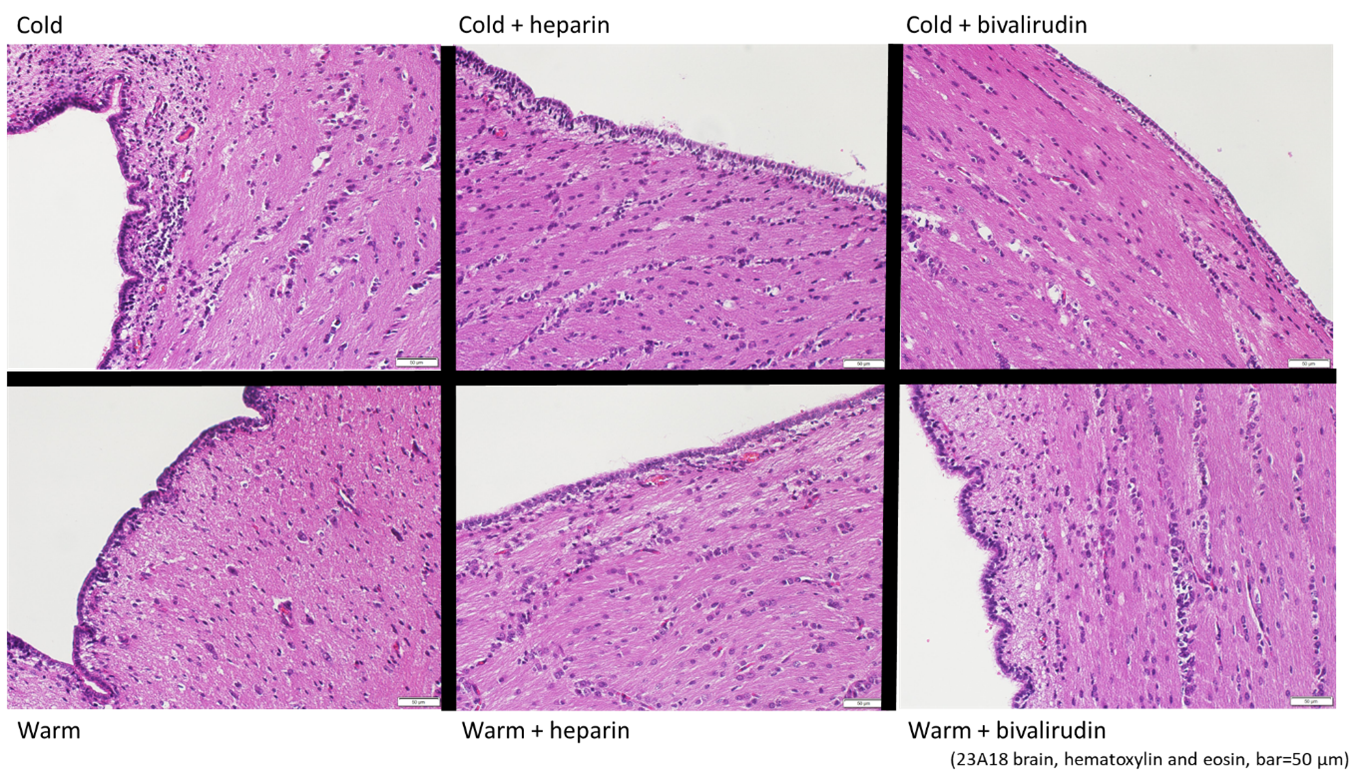
Brain blood flow
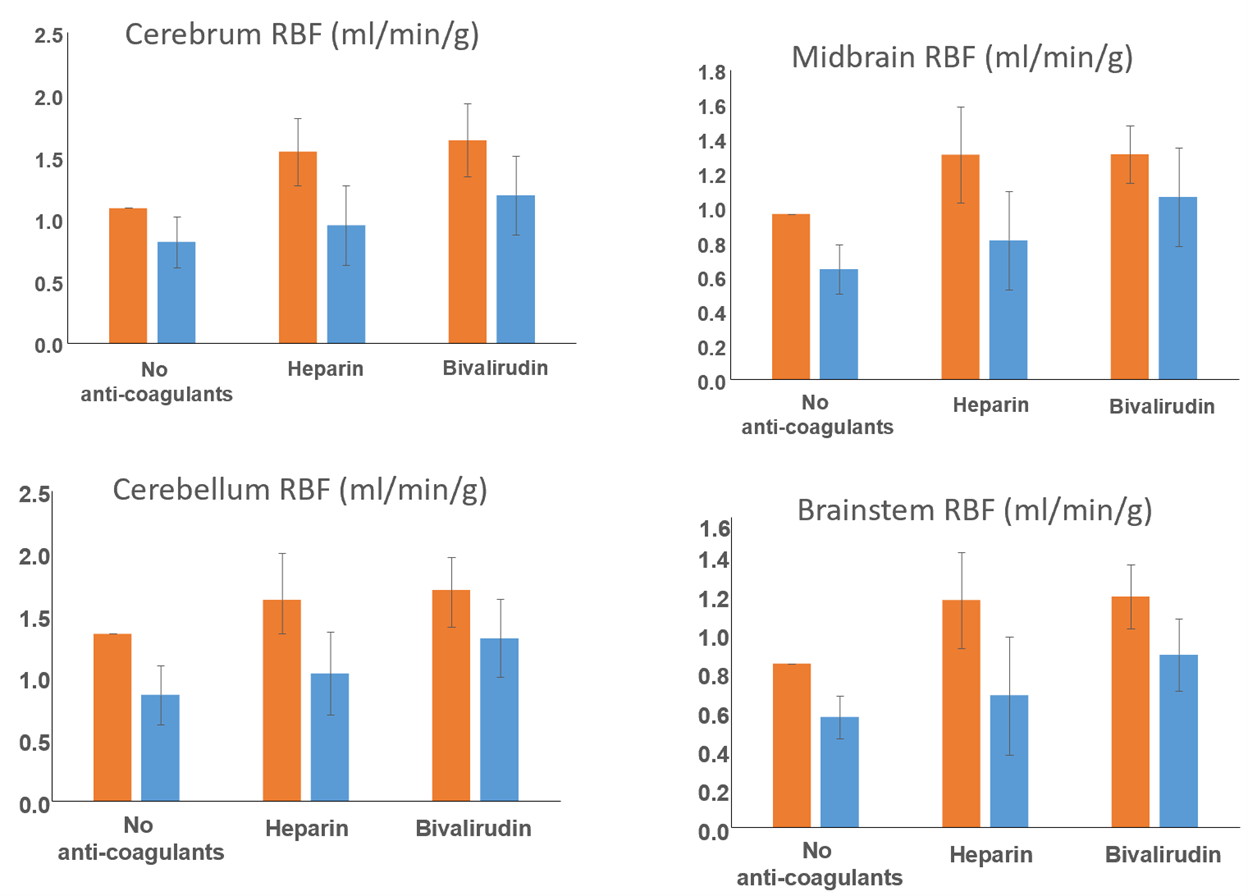
Representative histology images