Neonatal Quality Improvement 6
Session: Neonatal Quality Improvement 6
529 - A Quality Improvement Project Using a Factorial Design to Develop and Implement a Post-Partum Depression Screening Process in a Tertiary Level IV NICU
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 529.3801
Shelbye Schweinhart, University of Louisville School of Medicine, Louisville, KY, United States; Cynthia S. Crabtree, University of Louisville - Department of Pediatrics, Louisville, KY, United States; Shannon Evans, University of Louisville, Prospect, KY, United States; Claire Niehaus Milligan, University of Louisville School of Medicine, Louisville, KY, United States; Tamina Singh, University of Louisville School of Medicine, Louisville, KY, United States; Hannah Fischer, University of Louisville, Louisville, KY, United States

Shelbye Schweinhart, MD (she/her/hers)
Neonatal Fellow
University of Louisville School of Medicine
Louisville, Kentucky, United States
Presenting Author(s)
Background: Parental caregivers in the neonatal intensive care unit (NICU) have an increased risk for postpartum depression (PPD), often missing opportunities for recommended screening.
Objective: Our quality improvement team aimed to increase the percentage of maternal caregivers in a tertiary level IV NICU screened for PPD with a validated screening tool by 16 days of the child’s life from 0 to 90% in a 7-month period and connect those screening positive with psychosocial support.
Design/Methods: A factorial design was used to determine the ideal screening process in our unit, including the type of screen and method of delivery. Two levels for each factor were used. The Model for Improvement was used to study interventions including process standardization, electronic medical record (EMR) support, and data visualization. Data were displayed overtime on a control chart and stratified for race and language to ensure equitable delivery of the intervention. Sequential funnel plots by provider group were shared with team members overtime to provide feedback. Qualitative responses regarding the process were collected from frontline providers as a balancing measure.
Results: The Patient Health Questionaire-2 administered via phone or bedside interaction by the medical provider was the most reliable screening method in our context. EMR messaging showed a negative interaction regardless of screening type. PPD screening increased from 0% to a mean of 59% during our initial 7-month timeline. Importantly, 90% of positive screens were referred to our unit psychologist. Screening rates were similar comparing non-English speaking and non-white groups to the total population. Providers noted screening fit within their normal workflow and did not add significant time to daily patient care responsibilities.
Conclusion(s): Using a factorial design to develop a screening process for a busy tertiary NICU helped our team quickly identify the most effective screening method. The improvement in PPD screening rates was below our goal but resulted in a high percentage of patients receiving psychosocial support. Next steps include utilizing EMR prompts and other higher reliability interventions to improve our rates to >90% and screening additional caregivers.
P-Chart: Completed NICU Postpartum Depression Screens
.png) NICU postpartum depression screening increased from 0% to 59% over the initial project timeline. Key interventions are highlighted.
NICU postpartum depression screening increased from 0% to 59% over the initial project timeline. Key interventions are highlighted. Response Plots Comparing Type and Method for Postpartum Depression Screening
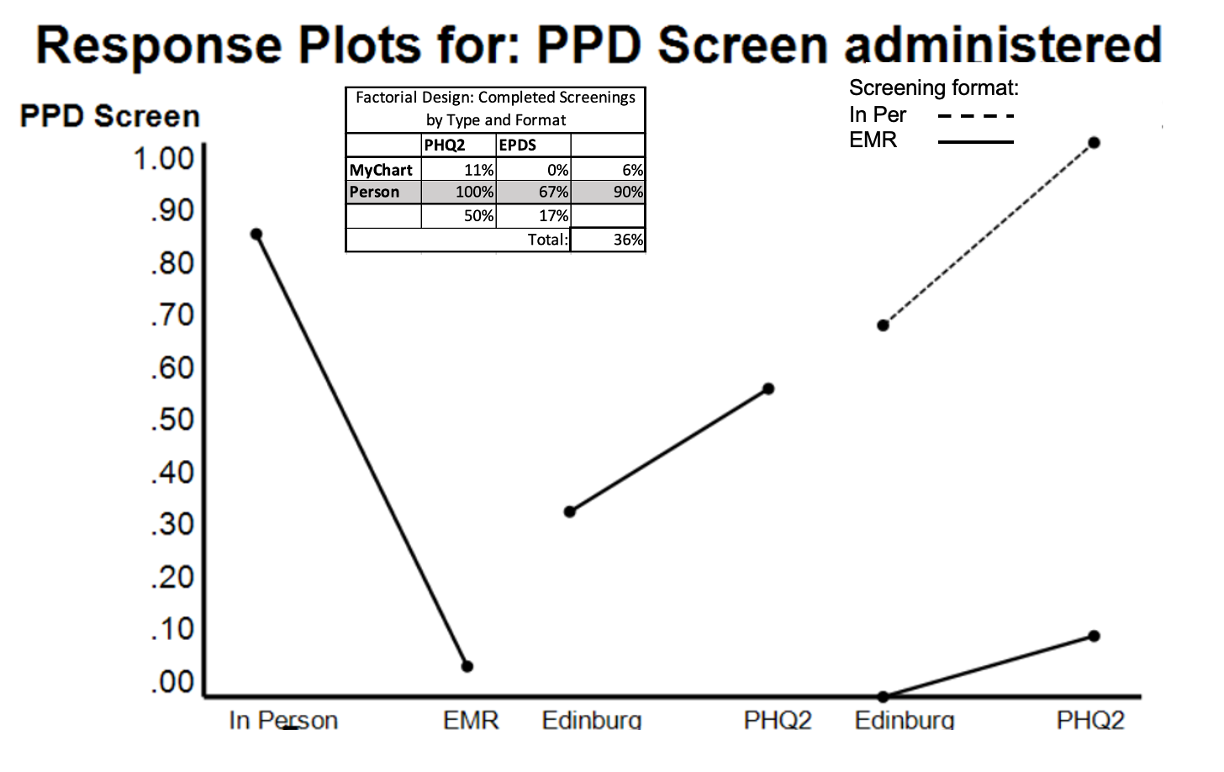 Our initial testing showed a significant negative effect of utilizing EMR communication to screen NICU caregivers without a significant effect of screener type. There was no significant interaction between factors tested.
Our initial testing showed a significant negative effect of utilizing EMR communication to screen NICU caregivers without a significant effect of screener type. There was no significant interaction between factors tested. Comparison of Postpartum Depression Screening Rates Across Segmented Groups
.png) Chart showing comparison of percentage of completed screens over time for total eligible to segmented groups. Overall, similar screening rates were achieved across groups.
Chart showing comparison of percentage of completed screens over time for total eligible to segmented groups. Overall, similar screening rates were achieved across groups. 

