Neonatal Quality Improvement 4
Session: Neonatal Quality Improvement 4
498 - 30-30-60 - A quality improvement project on faster enteral feed advancement and early fortification in a level IV neonatal intensive care unit
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 498.3865
Radhika Maddali, Montefiore Medical Center, Bayside, NY, United States; Carmen Alvarez Gell, The Children's Hospital at Montefiore, Bronx, NY, United States; Eric T. Basile, The Children's Hospital at Montefiore, Lynbrook, NY, United States; Jillian Connors, Albert Einstein College of Medicine, Bronx, NY, United States

Carmen A. Alvarez Gell, MD (she/her/hers)
Pediatric Resident
The Children's Hospital at Montefiore
Bronx, New York, United States
Presenting Author(s)
Background: Early nutrition for premature infants is a crucial determinant influencing postnatal growth, neurodevelopment, and survival. Feeding practices for preterm infants differ both within and between neonatal intensive care units (NICUs). Concerns about Necrotizing Enterocolitis (NEC) have historically led neonatal providers to delay the introduction of enteral feeding, slow advancement, and provide inadequate nutritional intake. However, these practices have not been shown to reduce the incidence of NEC. Instead, they increase the risk of morbidities such as dependence on total parenteral nutrition, liver injury, prolonged use of central lines, and central line-associated bloodstream infections, all of which are linked to worse long-term outcomes.
Objective: In infants born 27 0/7 to 32 6/7 weeks’ gestation, we aimed to shorten time to achieve full enteral feeds and decrease the duration of the central line usage by 20% from baseline.
Design/Methods: Infants born between 27 0/7 and 32 6/7 weeks' gestation were included. Infants who were small for gestational age (weighing less than the 10th percentile), had a birth weight of less than 1 kg, or had congenital gastrointestinal anomalies were excluded. A multidisciplinary quality improvement (QI) team identified key drivers (Figure 1) and developed change concepts followed by sequential “Plan, Do, Study, Act” (PDSA) cycles. To achieve our goals, we developed a simplified feeding guideline called 30-30-60, which involved initiation of enteral feeds at a volume of 30 ml/kg/day, advancement of feeds by 30 ml/kg/day, and earlier fortification of feeds at 60 ml/kg/day. Statistical control charts were utilized to study changes over time. The primary outcomes analyzed were days to full enteral feeds, central line days, and the number of peripherally inserted central catheter (PICC) placements. Balancing measures were rates of feeding intolerance and usage of donor breast milk.
Results: A total of 72 infants were included. The average time to achieve full enteral feeds decreased by 28%, from 11.3 days to 8.1 days (Figure 2), while the average duration of central line use decreased by 25%, from 8.4 days to 6.3 days (Figure 3). The percentage of infants requiring PICC placement decreased by 70%, from 37.2% at baseline to 11.3%. Episodes of feeding intolerance decreased over time, while the usage of donor human milk remained stable.
Conclusion(s): Quality improvement methodology was successfully utilized to implement new feeding guidelines, thereby reducing days to full enteral feeds and reducing central line days for very preterm neonates admitted to Level IV NICU.
Figure 1 - Key Driver Diagram
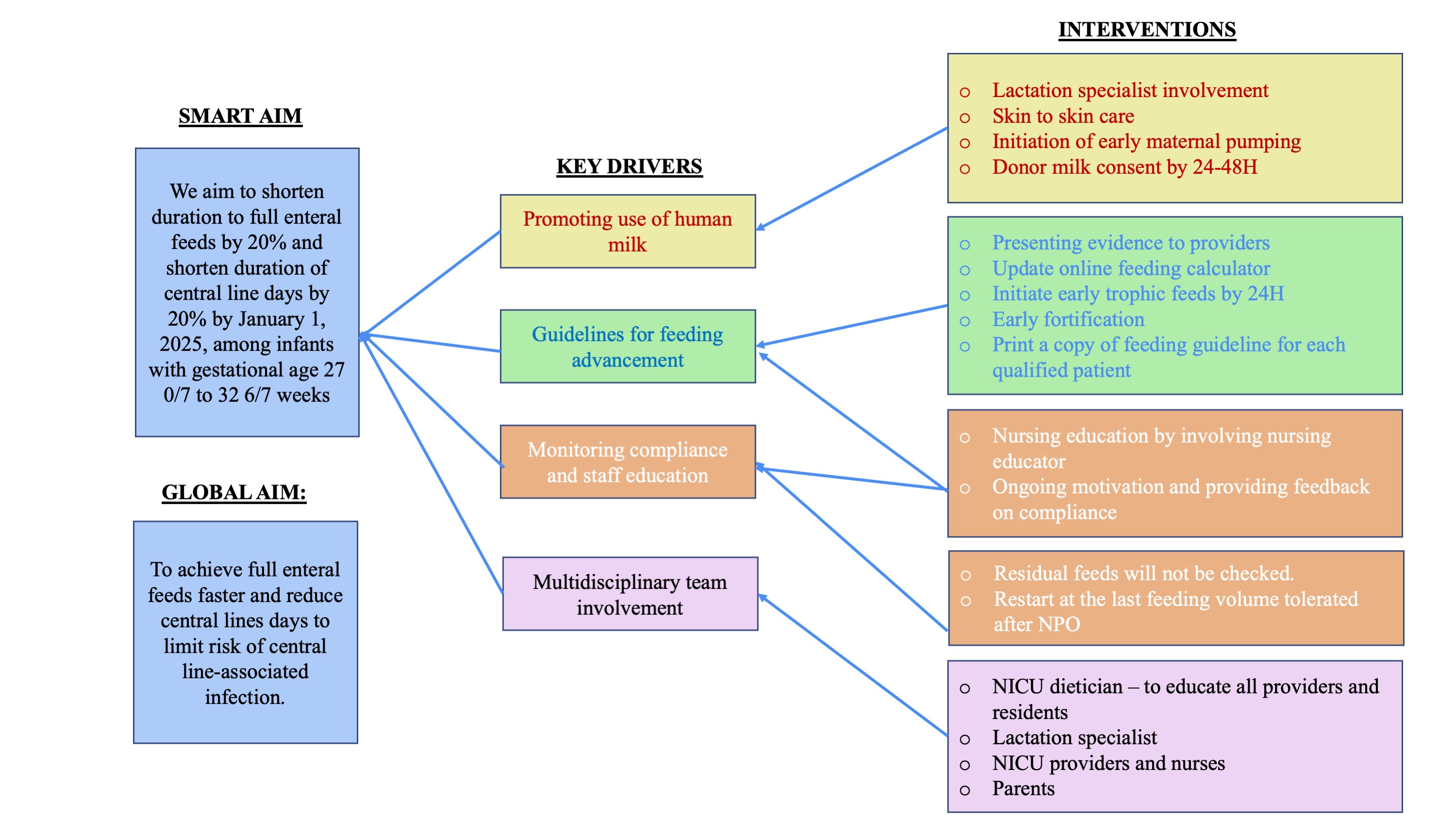
Figure 2 - Days to full enteral feeds
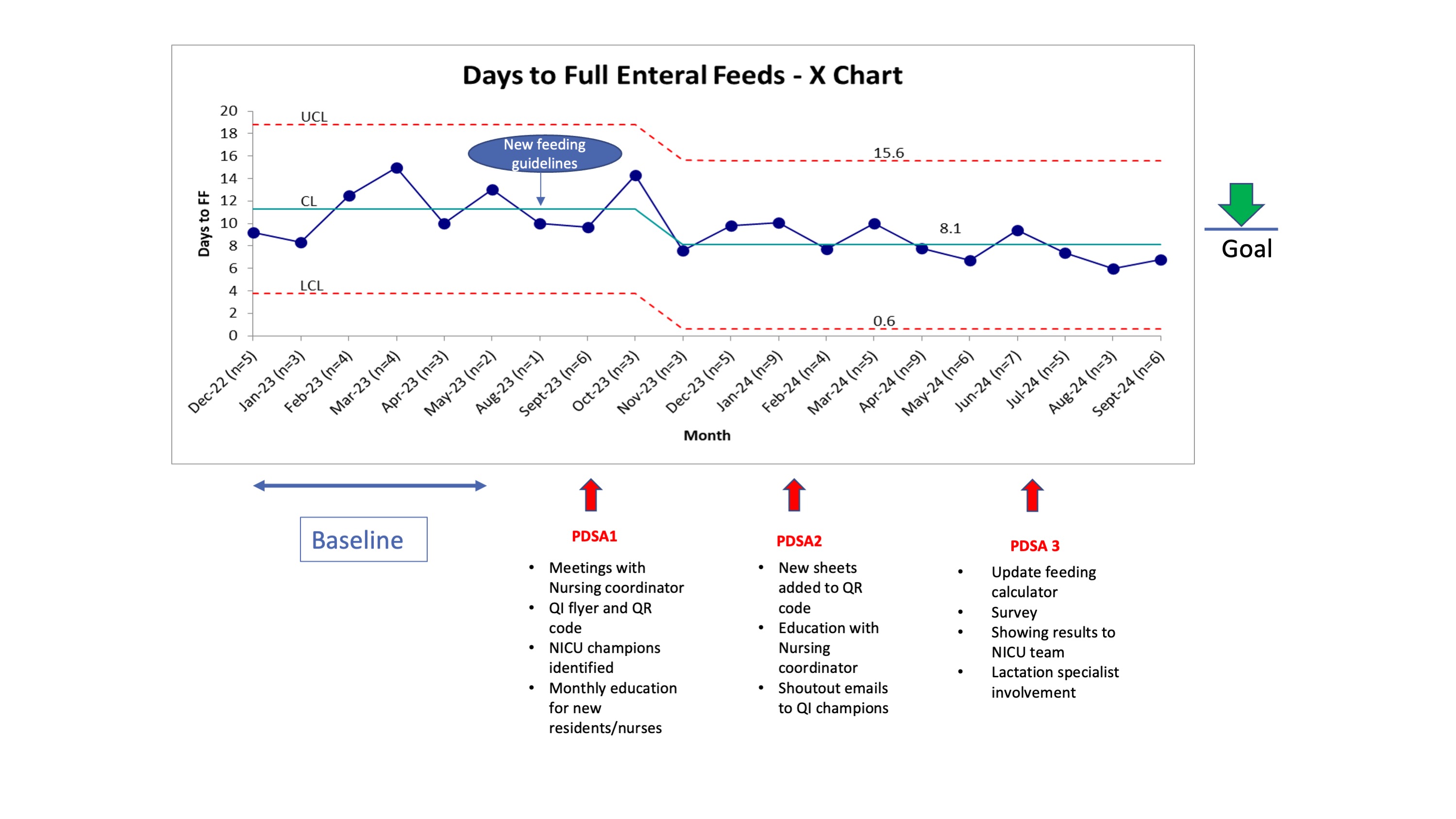 Statistical control chart of days to full enteral feeds by month with shift from baseline of a mean (blue center line) of 11.3 days per eligible infant to 8.1 days (28% decrease from baseline). UCL=upper control limit, LCL=lower control limit.
Statistical control chart of days to full enteral feeds by month with shift from baseline of a mean (blue center line) of 11.3 days per eligible infant to 8.1 days (28% decrease from baseline). UCL=upper control limit, LCL=lower control limit.Figure 3 - Central line days
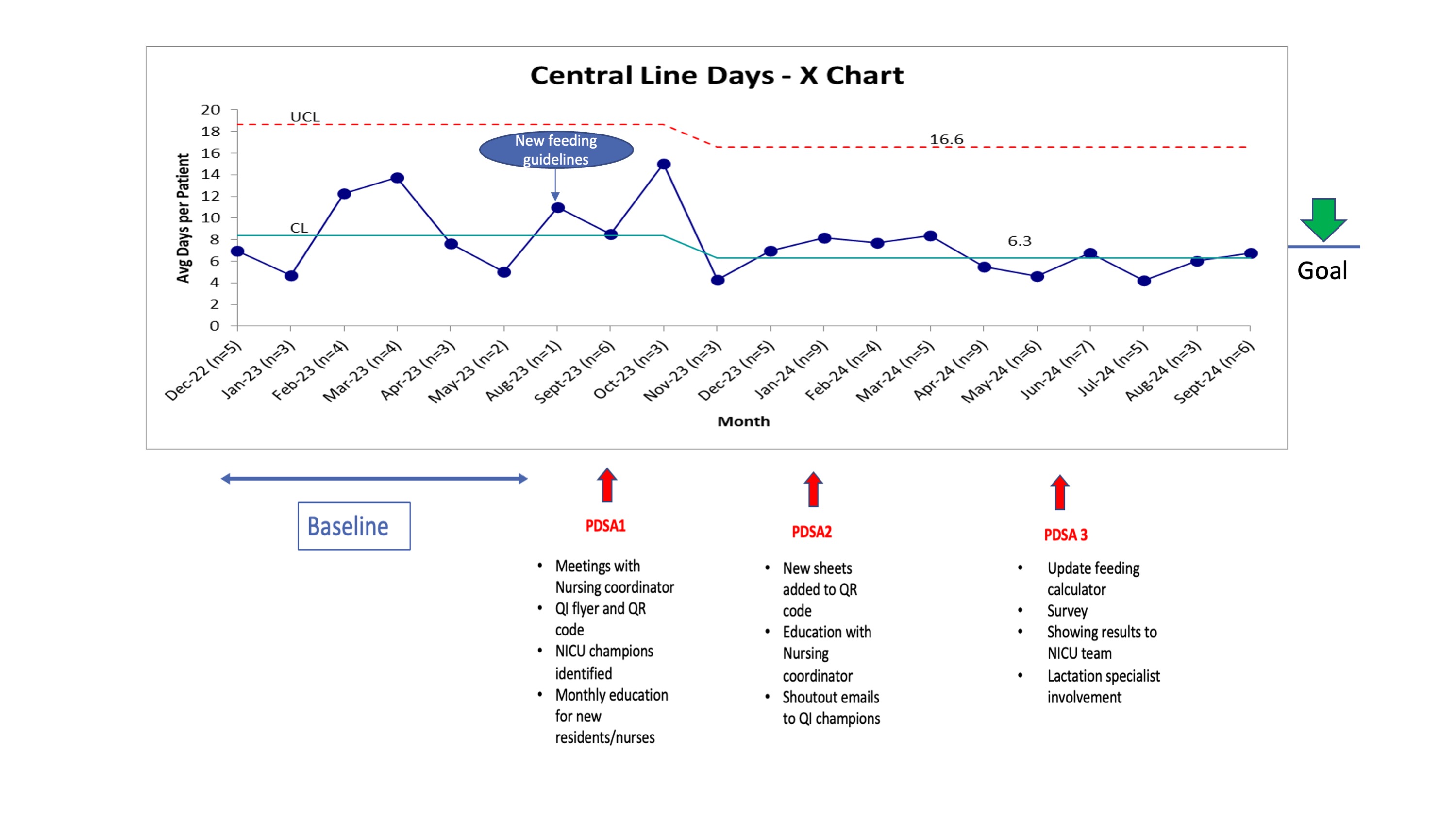 Statistical control chart of central line days by month with shift from baseline of a mean (blue center line) of 8.4 days per eligible infant to 6.3 days (25% decrease from baseline).
Statistical control chart of central line days by month with shift from baseline of a mean (blue center line) of 8.4 days per eligible infant to 6.3 days (25% decrease from baseline). 

