Emergency Medicine 5
Session: Emergency Medicine 5
260 - A taxonomy of intubation errors in pediatric emergency intubations
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 260.3765
Abha Athale, Nationwide Children's Hospital, Columbus, OH, United States; Jennifer Mitzman, Nationwide Children's Hospital, Columbus, OH, United States; Sarah Chen, Nationwide Children's Hospital, Columbus, OH, United States; Ambrish B. Patel, Nationwide Children’s Hospital, Powell, OH, United States; Anne Runkle, Ohio State University College of Medicine, Columbus, OH, United States
- AA
Abha Athale, DO, MSc (she/her/hers)
Pediatric Emergency Medicine Attending Physician
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Intubation is an infrequent but critical procedure in the Pediatric Emergency Department (PED). Compared to adult intubations, pediatric intubations (PI) have additional anatomic and physiologic challenges. PIs are optimally completed in under 45 seconds, giving a time restraint challenge. Recording video laryngoscopy (VL) gives an opportunity to review intubations and identify areas for improvement. Adult airway literature reports a classification system for intubation errors which provides structure for video review-based quality assurance (QA). There is no system for PIs.
Objective: We aim to modify an existing taxonomy of intubation errors to reflect those encountered during PI and determine the frequency of each in successful and unsuccessful attempts.
Design/Methods: This prospective, observational study uses a convenience sample of successive, de-identified, recorded PI attempts. Error definitions were developed after review of a pilot video set. Subsequent videos were coded by 2 independent reviewers with adjudication from a 3rd. Summary statistics were used to quantify error prevalence. Interrater reliability was measured by Cohen’s Kappa. Fisher’s exact and Mann-Whitney tests compared errors of successful and unsuccessful attempts.
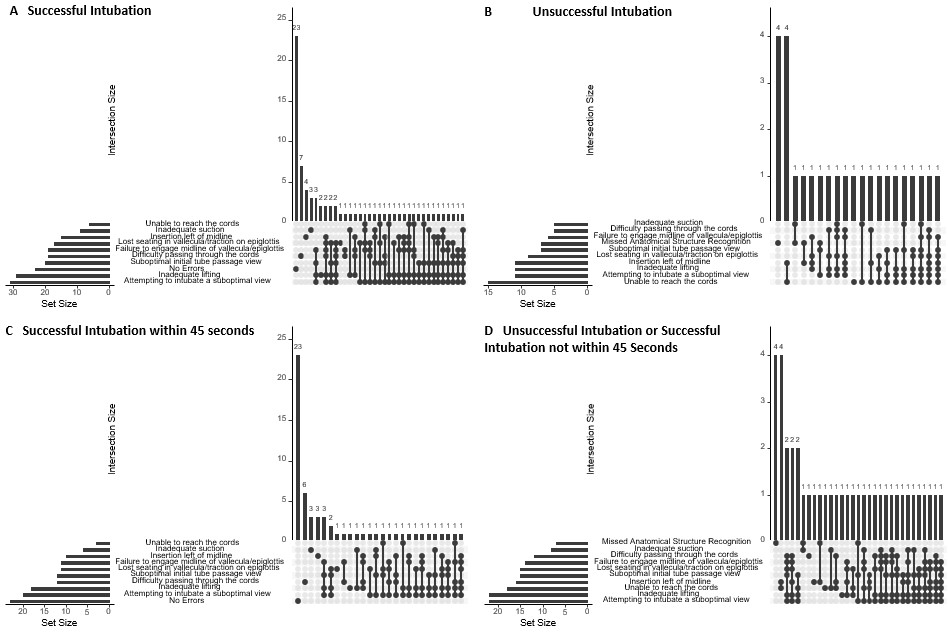
Results: One hundred sequential videos were reviewed. Ten of 14 intubations errors had a Cohen’s Kappa 0.6 or more, indicating substantial agreement. The most common errors were attempting endotracheal tube (ETT) passage with a suboptimal view (42%), inadequate lifting (40%), blade insertion left of midline (26%), losing traction (26%), failure to engage midline structures (25%), and difficulty passing through the vocal cords (24%) [Table 1]. Seventy four attempts were successful, with a median of 1 (Inter Quartile Range (IQR) 0-4) error; unsuccessful attempts had a median of 3 (IQR 2-5) errors (p=0.01). Sixty attempts were successful under 45 seconds; of these, 35 (58%) had 0 or 1 error. All errors in the insertion phase (insertion left of midline, overly deep insertion, and missed anatomical structure recognition), and inability to reach the cords with the ETT, were significant between successful and unsuccessful attempts (p < 0.05). For successful intubations under 45 seconds, inadequate lifting, losing traction, and attempting to intubate a suboptimal view were also significant (p < 0.05) [Table 2].
Conclusion(s): This study describes a system to classify errors during pediatric VL intubation and identifies their frequency in a PED. These classifications can be used to develop a standard intubation QA process, inform trainee education, and provide individual coaching.
Table 1. Intubation video review errors identified and overall success rates.
1.jpeg
Table 2. Errors between intubation attempts that were successful in 45 seconds versus unsuccessful or successful in more than 45 seconds
Table 2. errors successful vs unsuccessful.jpeg
Figure 1. Upset diagrams depicting errors based on intubation success