Mental Health 2
Session: Mental Health 2
778 - Postpartum Depression among Newly Delivered Mothers based on Kangaroo Mother Care and Neonatal Disease Severity
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 778.6361
Herbert Kapesa, Center for Infectious Disease Research in Zambia, Lusaka, Lusaka, Zambia; Kevin Owuor, University of Alabama at Birmingham, Birmingham, AL, United States; J Anitha Menon, Curtin University Dubai, Dubai, Dubai, United Arab Emirates; Waldemar Carlo, UAB School of Medicine, Birmingham, AL, United States; Albert Manasyan, University of Alabama School of Medicine, Birmingham, AL, United States; Jyoti Lakhwani, Centre for Infectious Disease Research in Zambia, Lusaka, Lusaka, Zambia

Jyoti Lakhwani, MD, PGD Neonatology, MPH/MHLM (she/her/hers)
Fellow
Centre for Infectious Disease Research in Zambia
Lusaka, Lusaka, Zambia
Presenting Author(s)
Background: Postpartum Depression (PPD) is a serious public health problem affecting 17.2% of women globally, with higher rates recorded in southern Africa – 39.9%. Admission of a neonate to the neonatal intensive care unit (NICU) is a risk factor for PPD.
Objective: Our objective is to determine the association between the location of treatment for their newborn with the prevalence of maternal PPD.
Design/Methods: We conducted a cross-sectional study among newly delivered mothers at the Women and Newborn Hospital – University Teaching Hospitals in Lusaka, Zambia between June 2022 – May 2023. Mothers of infants discharged home from the Postnatal Ward (normal newborn nursery), NICU, or Kangaroo Mother Care (KMC) Ward after NICU admission were screened for PPD using the Edinburgh Postnatal Depression Scale (EPDS) screening tool at 6-8 weeks postnatally. Mothers who scored 11+ were categorized as having possible PPD. Poisson models were used to estimate risk ratios (RR) for differences in PPD positivity in the study arms. The primary outcome was PPD following KMC versus NICU discharge in models adjusted for maternal age, BMI, parity, gravida, mode of delivery, marital status, HIV status, level of education, source of income, baby sex, and birth weight.
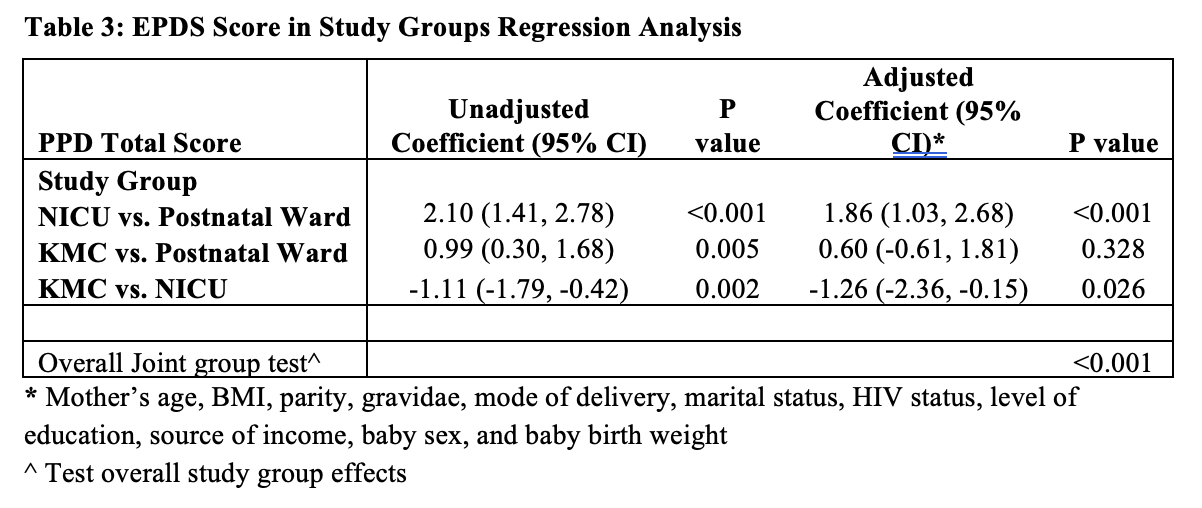
Results: We screened 1056 newly delivered women for PPD pooled from mother-infant pairs discharged from the Postnatal Ward (n=352), KMC Ward (n=352), or NICU (n=352). Overall, the average age of the mothers was 27.5 years, 61.1% had secondary education, 59.2% were unemployed, 80.7% were married, and 11.2% were HIV-positive (Table 1). Mothers whose newborns were discharged from the KMC Ward after NICU had a lower rate of PPD (21.3%) compared to those directly discharged from the NICU (29.0%) (p < 0.001) (Table 2). In adjusted analysis, KMC had a lower EPDS score of -1.26 (95% CI -2.36, -0.15) when compared to NICU in the adjusted analyses (p=0.026) (Table 3).
Conclusion(s): Discharge home from the KMC Ward following the NICU is associated with a lower rate of PPD among newly delivered mothers compared to direct NICU discharge and eliminated the difference in EPDS scores between Postnatal Ward and NICU admission.
Table 1: Maternal and Newborn Characteristics
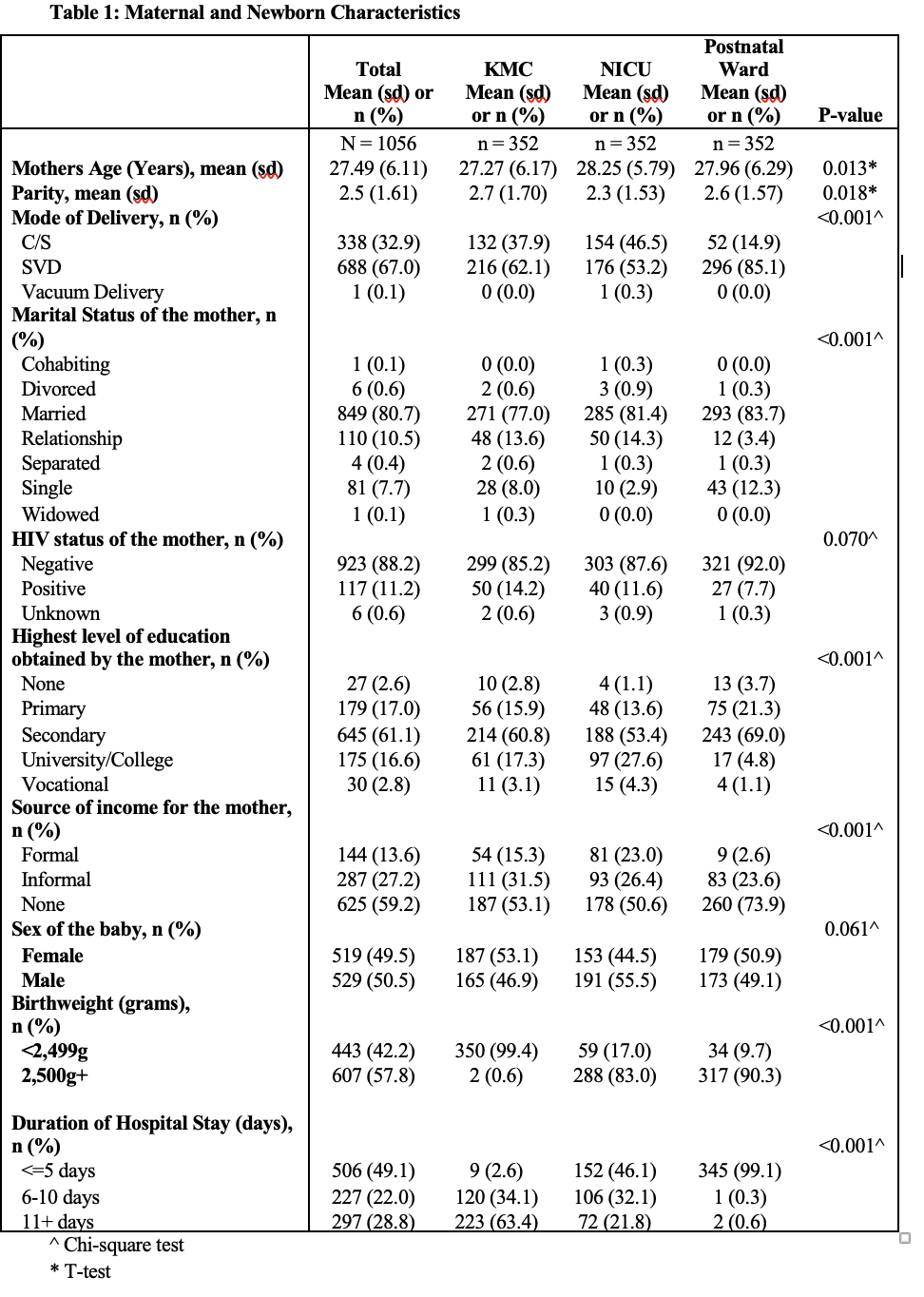
Table 2: Maternal EPDS and Anxiety Outcomes
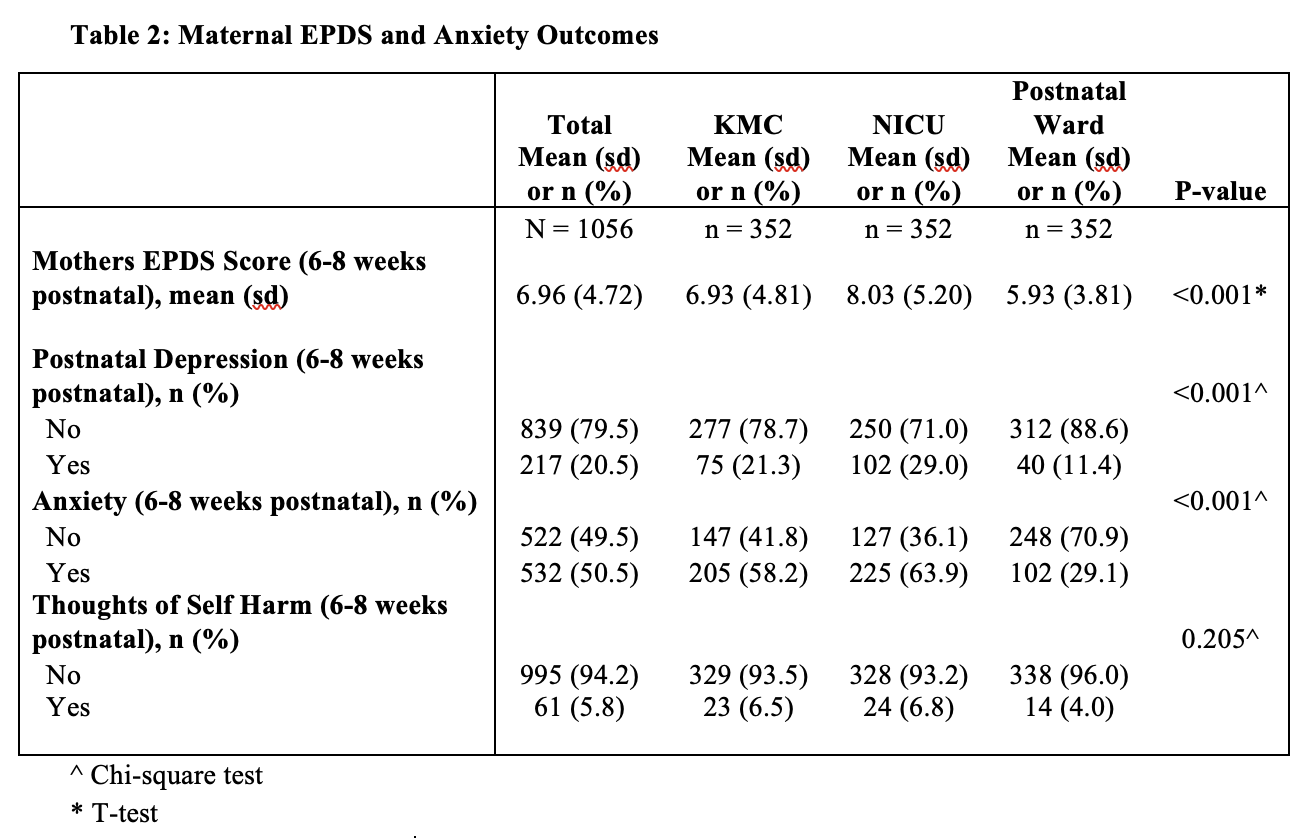
Table 3: EPDS Score in Study Groups Regression Analysis