Hematology/Oncology 2: Pediatric Hematology
Session: Hematology/Oncology 2: Pediatric Hematology
116 - Procalcitonin Elevation in Patients with Sickle Cell Disease (SCD) Hospitalized for Vaso-Occlusive Pain Episodes (VOE)
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 116.6372
Giorgi Maziashvili, Emory University School of Medicine, Atlanta, GA, United States; Rawan Korman, Emory University School of Medicine, Atlanta, GA, United States; Dunia Hatabah, Emory University School of Medicine, Atlanta, GA, United States; LOU ANN S. BROWN, Emory University, Atlanta, GA, United States; Frank Harris, Emory University, Atlanta, GA, United States; Chris A. Rees, Emory University School of Medicine, Atlanta, GA, United States; Carlton Dampier, Emory University School of Medicine, Atlanta, GA, United States; Claudia R.. Morris, Emory University School of Medicine, Atlanta, GA, United States
.jpg)
Rawan Korman, MD (she/her/hers)
Postdoctoral Research Fellow
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: Procalcitonin (PCT) is a plasma biomarker that helps distinguish serious bacterial infection (SBI) from other causes of inflammation or viral illnesses. Patients with SCD are more prone to bacterial infections due to functional asplenia. During VOE with fever, it is often hard to distinguish the fever source leading to empiric antibiotic use for all patients. The role of PCT in children with SCD-VOE remains unknown.
Objective: Assess the relationship between PCT levels & fever, ACS and other variables in children with SCD-VOE.
Design/Methods: Secondary analysis of samples from a pharmacokinetics/pharmacodynamics study & Phase-2 randomized controlled trial of intravenous arginine therapy in patients age 3-21 years with SCD-VOE. Plasma PCT was measured at emergency department (ED) presentation & hospital discharge (DC). Non-SCD studies of bacteremia risk define PCT≥0.5 ng/mL as elevated & ≥2ng/mL high risk. Associations between clinical and lab variables with PCT were determined via pearson correlation and unpaired t-test as appropriate.
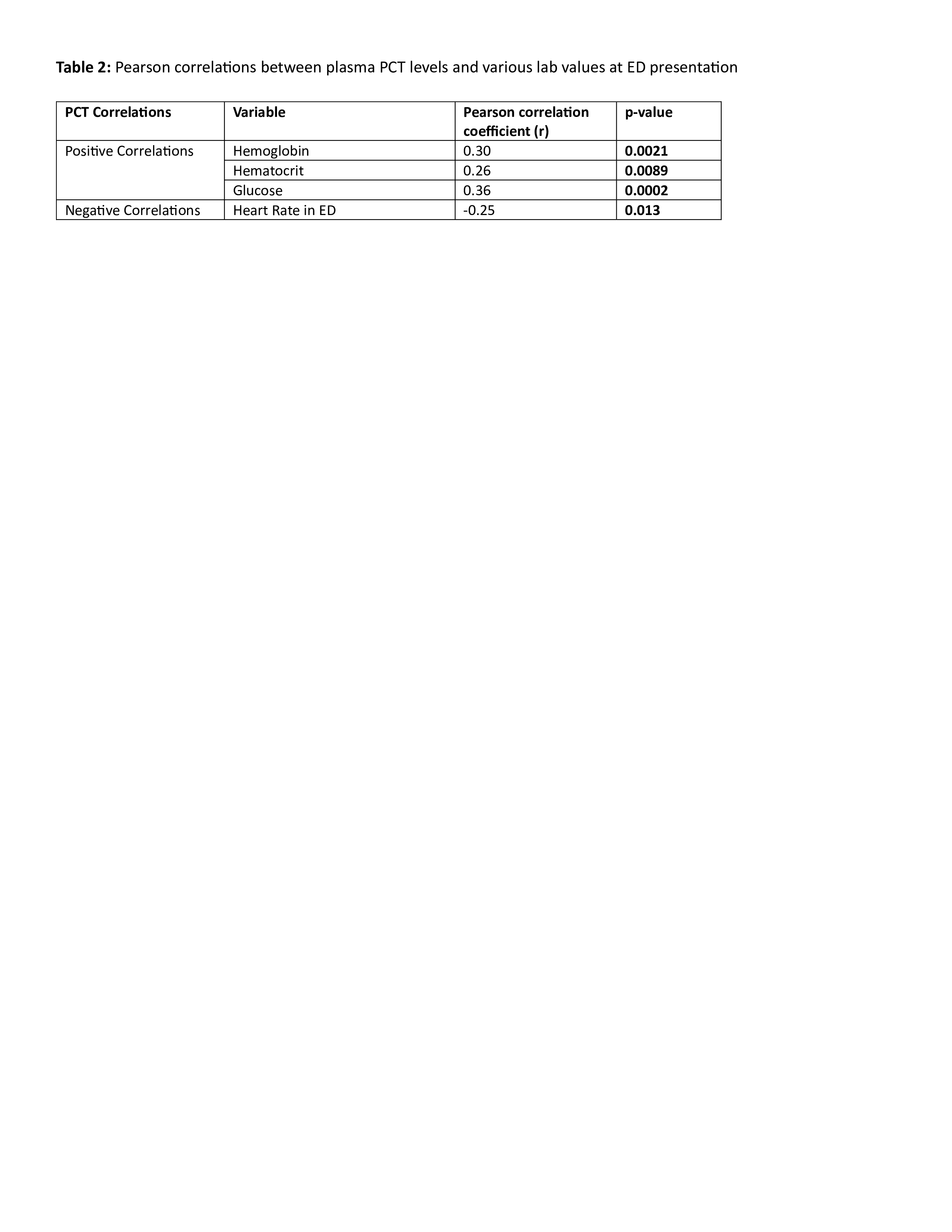
Results: 102 patients (13±4 years, 49% male, 66% HbSS, 68% on HU) were included. 14% had fever ≥38.0ºC in the ED, 18% developed fever during hospital stay & 11 presented with (n=3) or developed (N=8) ACS. PCT was elevated≥0.5 ng/mL in 69%, with 9% at high risk (Table1). Among the 70 patients with elevated PCT, 14% had fever in the ED & an additional 18% developed fever during the hospital stay, 46% had chest pain (CP) & 9% had ACS, similar to patients with normal PCT levels. Higher creatinine was the only difference (p < 0.05) among patients with PCT≥2ng/mL vs PCT < 0.5ng/mL. PCT did not significantly decrease by DC, with DC levels remaining elevated in 60%. PCT positively correlated with hemoglobin (r=0.30,p=0.002) & glucose (r=0.36,p < 0.001) but not white blood cell count (WBC; r=0.02,p=0.88).
Conclusion(s): PCT levels are elevated in the majority of patients with SCD-VOE, reflecting a systemic inflammatory response that persists at DC & is unrelated to bacterial infection. In our cohort, PCT elevation did not correlate with fever, ACS/pneumonia, CP, WBC or other relevant clinical/demographic factors. However no patients had bacteremia or SBI. While PCT shows promise for antibiotic stewardship in healthy populations, its predictive value in SCD require more research; baseline ranges & SBI thresholds likely differ from the general population & need to be defined in large prospective studies of SCD-fever. Although the role of PCT to identify SBI risk in SCD is unclear, PCT levels < 0.5ng/mL may suggest low risk, potentially allowing for antibiotic stewardship in the future.
Demographics, clinical characteristics, and laboratory values in patients with PCT ≥ 2, ≥ 0.5, and <0.5
.jpg)
Pearson correlations between plasma PCT levels and various lab values at ED presentation