Neonatal Nephrology/AKI 1
Session: Neonatal Nephrology/AKI 1
010 - Post-Operative Acute Kidney Injury in Surgical Neonates: A Secondary Analysis of the ADVANCE Cohort
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 10.6393
Matthew C. Gillen, Emory University School of Medicine, Atlanta, GA, United States; Jennifer Rumpel, Arkansas Children's Hospital, Little Rock, AR, United States; Corey Nagel, University of Arkansas for Medical Sciences, Little Rock, AR, United States; Jonathan Bona, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Mario Schootman, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Daniel Liu, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Sofia I. Perazzo, Childrens National Hospital, North Bethesda, MD, United States; Mary E. Revenis, Children's National Health System, Chevy Chase, MD, United States; Semsa Gogcu, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Andrew M. South, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Tahagod Mohamed, Nationwide Children's Hospital, Columbus, OH, United States; Elizabeth Bonachea, Nationwide Children's Hospital, Columbus, OH, United States; Matthew W. Harer, University of Wisconsin School of Medicine and Public Health, Waunakee, WI, United States; Thomas Nienaber, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Mona Khattab, Baylor College of Medicine, Houston, TX, United States; Catherine Joseph, Baylor College of Medicine, Houston, TX, United States; Eileen A. Ciccia, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Tasnim Najaf, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Michelle Starr, Indiana University School of Medicine, Indianapolis, IN, United States; Rachel Han, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States; Cara Slagle, Indiana University School of Medicine, Indianapolis, IN, United States
- MG
Matthew C. Gillen, MD
Pediatric Nephrology Fellow
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: Acute kidney injury (AKI) affects about one-third of critically ill neonates and is independently associated with increased morbidity and mortality. Less is known about post-operative AKI, AKI after surgical procedures, and how post-operative AKI affects neonatal morbidity and mortality.
Objective: To describe the epidemiology of post-operative AKI in a large, multicenter cohort of neonates undergoing surgical procedures and to characterize the relationship between post-operative AKI and mortality.
Design/Methods: We performed a secondary analysis of the ADVANCE database, a cohort of 44,689 patients admitted to ten Level IV neonatal intensive care units (NICUs) in the Children’s Hospitals Neonatal Consortium between 2011 and 2023. If a patient had multiple surgeries only the first surgical procedure was evaluated. We included infants with measured serum creatinine during both the 7 day preoperative period and 14 day postoperative period. Infants with AKI immediately prior to surgery were excluded. The primary outcome was post-operative AKI, defined as AKI occurring within 14 days of surgery based on neonatal modified Kidney Disease: Improving Global Outcomes (KDIGO) serum creatinine only criteria. Secondary outcomes were length of stay and in-hospital mortality.
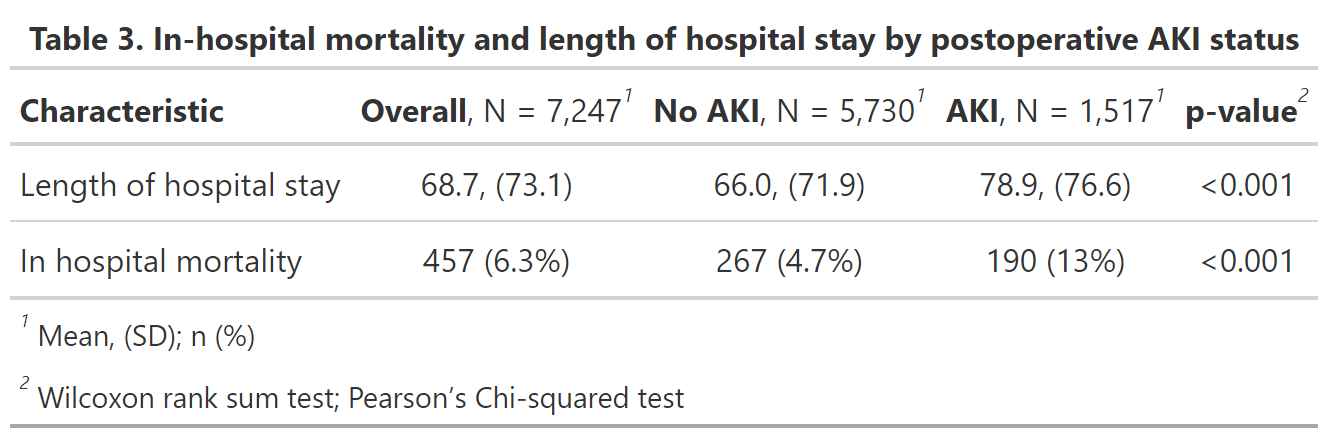
Results: In total, 10,886 neonates underwent surgical procedures. 3,639 patients were excluded (33.4%), and 7,247 patients met inclusion criteria. Fifty-seven percent of patients (n = 4,113) were male (Table 1). Median gestational age at birth was 35.4 weeks (IQR 27.7 to 38.3), and median corrected gestational age at surgery was 38.1 weeks (IQR 34.3 to 40.6). Median birthweight (BW) was 2.3kg (IQR 1.0 to 3.1 kg). Sixteen percent (n = 1,135) and 21% (n = 1,517) of patients developed AKI within 7 and 14 days, respectively. Of patients who developed post-operative AKI within 14 days, 9.3% (n = 672) were Stage 1 AKI while 11.6% (n = 845) were Stage 2 or 3 AKI (Table 2). Compared to neonates without post-operative AKI, neonates with post-operative AKI had longer hospital stays (66.0 vs 78.9 days; p< 0.001) and higher rates of in-hospital mortality (4.7% vs. 13%; p< 0.001) (Table 3).
Conclusion(s): Post-operative AKI is estimated to occur in about 1 in 5 neonates undergoing surgical procedures and is associated with greater in-hospital mortality and longer length of stay. Future work includes the identification of peri-operative risk factors associated with post-operative AKI in this heterogenous population.
Table 1. Patient characteristics
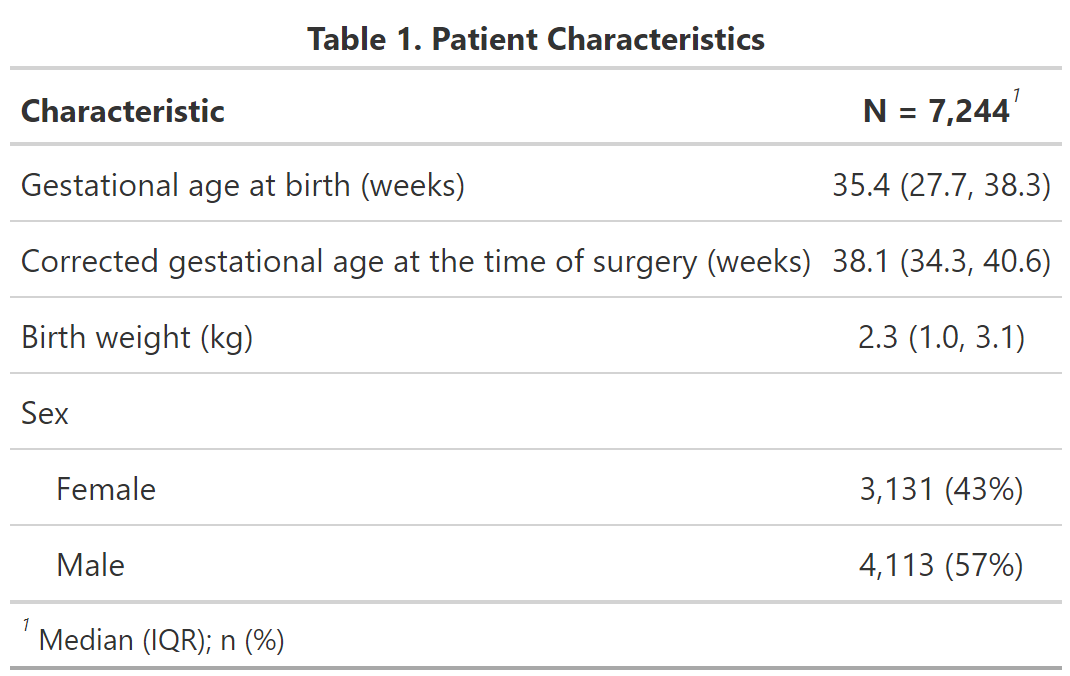
Table 2. Maximum AKI stage in the 2 week postoperative period stratified by corrected gestational age
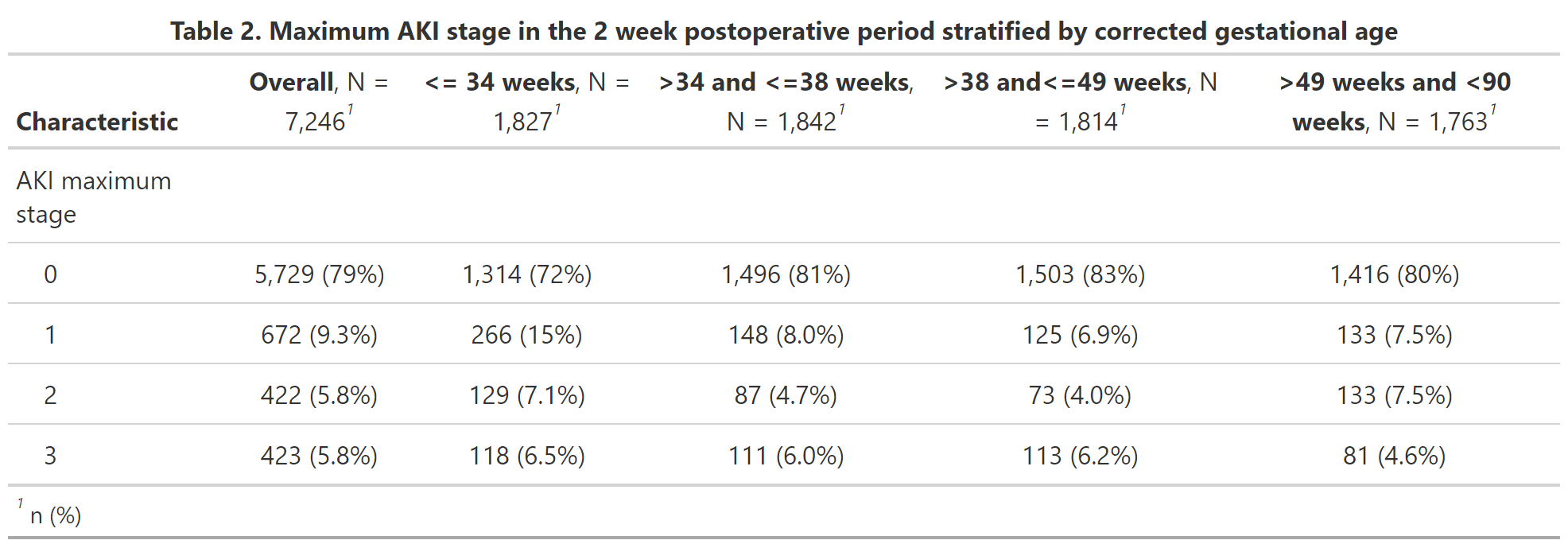
Table 3. In-hospital mortality and length of hospital stay by postoperative AKI status