Medical Education 3: Simulation
Session: Medical Education 3: Simulation
201 - Assessment of the Proficiency and Comfort Level of Pediatrics Residents Certified as Stop the Bleed Instructors: A Novel Use of Simulation
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 201.3623
Bradley Yingst, Dell Children's Medical Center of Central Texas, Austin, TX, United States; Guyon Hill, University of Texas at Austin Dell Medical School, Austin, TX, United States; Ada Earp, University of Texas at Austin Dell Medical School, Austin, TX, United States; Elizabeth Y. Vezzetti, Texas Christian University, Fort Worth, TX, United States; Robert Vezzetti, UT Dell Medical School/Dell Children's Medical Center, Austin, TX, United States

Bradley Yingst, DO
Pediatric Emergency Medicine Fellow
Dell Children's Medical Center of Central Texas
Austin, Texas, United States
Presenting Author(s)
Background: Trauma is a leading cause of pediatric deaths. The Stop the Bleed® Campaign (STB) is designed to teach hemorrhagic control for trauma victims. Using simulation, we investigate the proficiency and comfort level of utilization of Stop the Bleed® techniques among pediatric residents. The potential positive impact that a pediatrician certified as a Stop the Bleed® instructor would have in their community throughout their career should be recognized and we have adopted this program of instruction as part of our pediatric residency simulation curriculum.
Objective: We trained and certified all pediatrics residents as STB instructors. Additionally, we obtained pre- and post-training surveys assessing comfort with the material and knowledge obtained. We then conducted follow-up simulation training to assess skill retention.
Design/Methods: All pediatric residents at our facility completed the STB course and were certified as instructors. Pre and post surveys were used to assess knowledge of and confidence in methods of hemorrhage control taught through the STB course. We then performed follow-up simulation scenario testing one year after the initial course completion. The simulations consisted of a 7-year-old struck by a car with lower leg arterial bleeding and a 13-year-old stabbing victim. We also conducted post-simulation assessment of the use of proper STB techniques and resident confidence in using STB techniques. Our goal was to assess proper application of tourniquets and pressure dressings according to standardized STB teaching and reassess resident comfort and skill retention.
Results: In the initial training and certification period, we captured 59/64 residents for a 92.1% participation rate. Our pre and post survey rate was 83%. Our surveys showed a marked increase in the acquisition of hemorrhage control skills and comfort in performing them. We performed two follow-up dedicated trauma simulations one year later that involved 61/68 available residents for a 98.7% participation rate that yielded an 82% survey rate. All but one group successfully placed a tourniquet in less than 5 minutes and all groups successfully packed the wound. The only group not able to successfully complete the simulation requiring a tourniquet was composed primarily of untrained new interns.
Conclusion(s): This study demonstrated that using simple simulation techniques and equipment, pediatric residents trained in Stop the Bleed® techniques showed significant increases in both their knowledge and comfort level with performing hemorrhage control. We propose Stop the Bleed® should be a part of pediatric residency training.
Figure 1
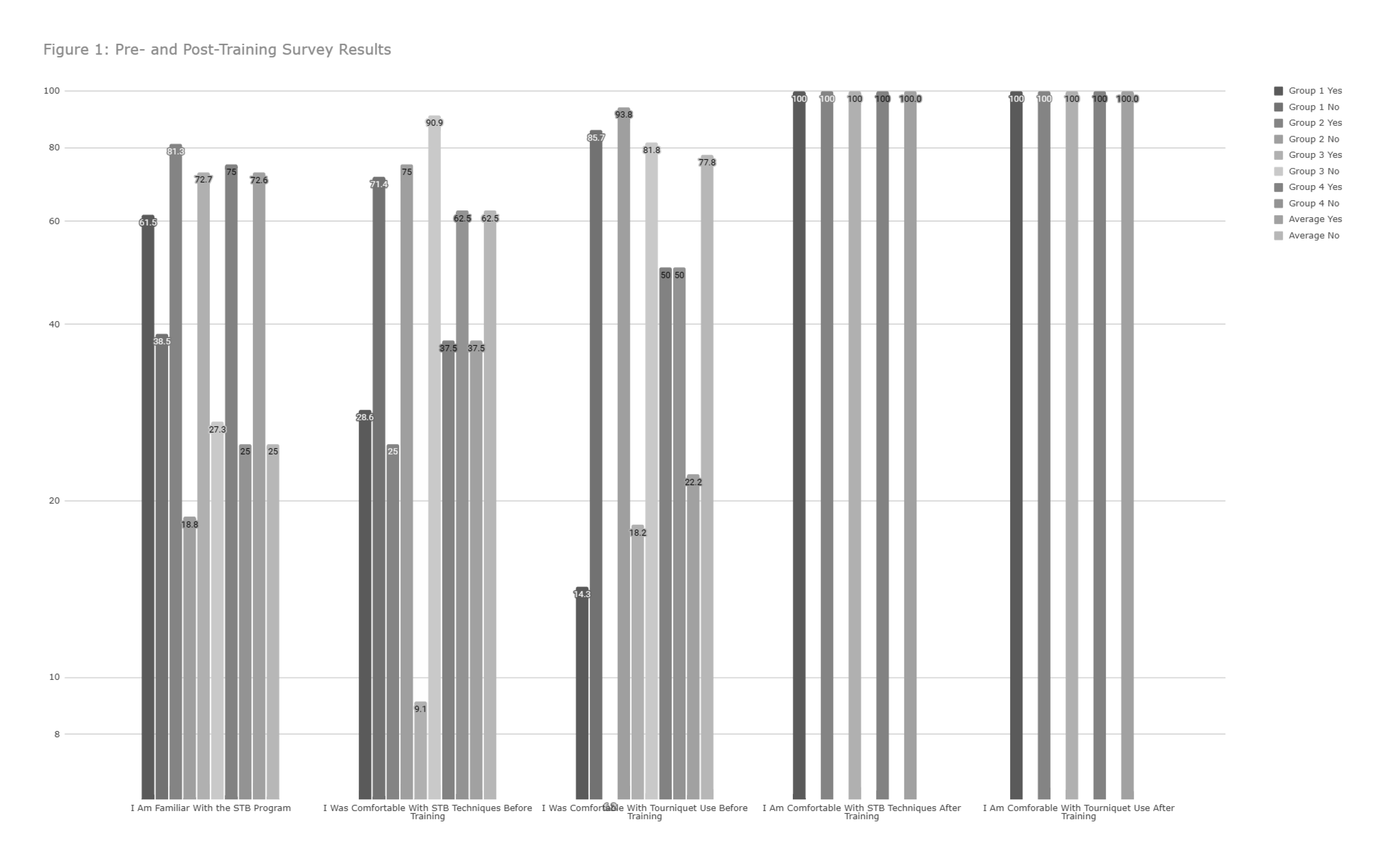 Pre- and Post-Training Survey Results
Pre- and Post-Training Survey Results Figure 2
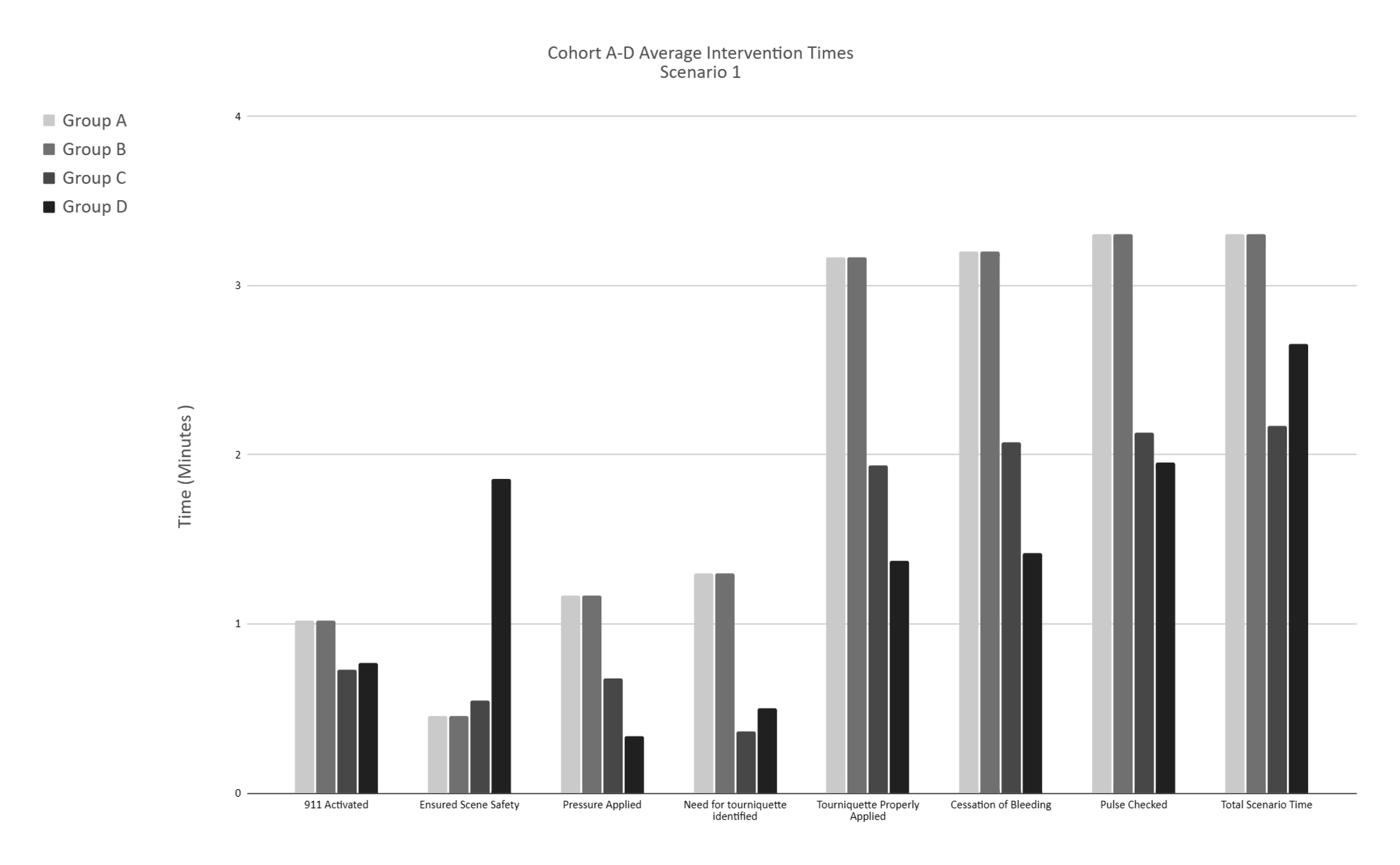 Cohort A-D Average Intervention Times, Scenario 1
Cohort A-D Average Intervention Times, Scenario 1Figure 3
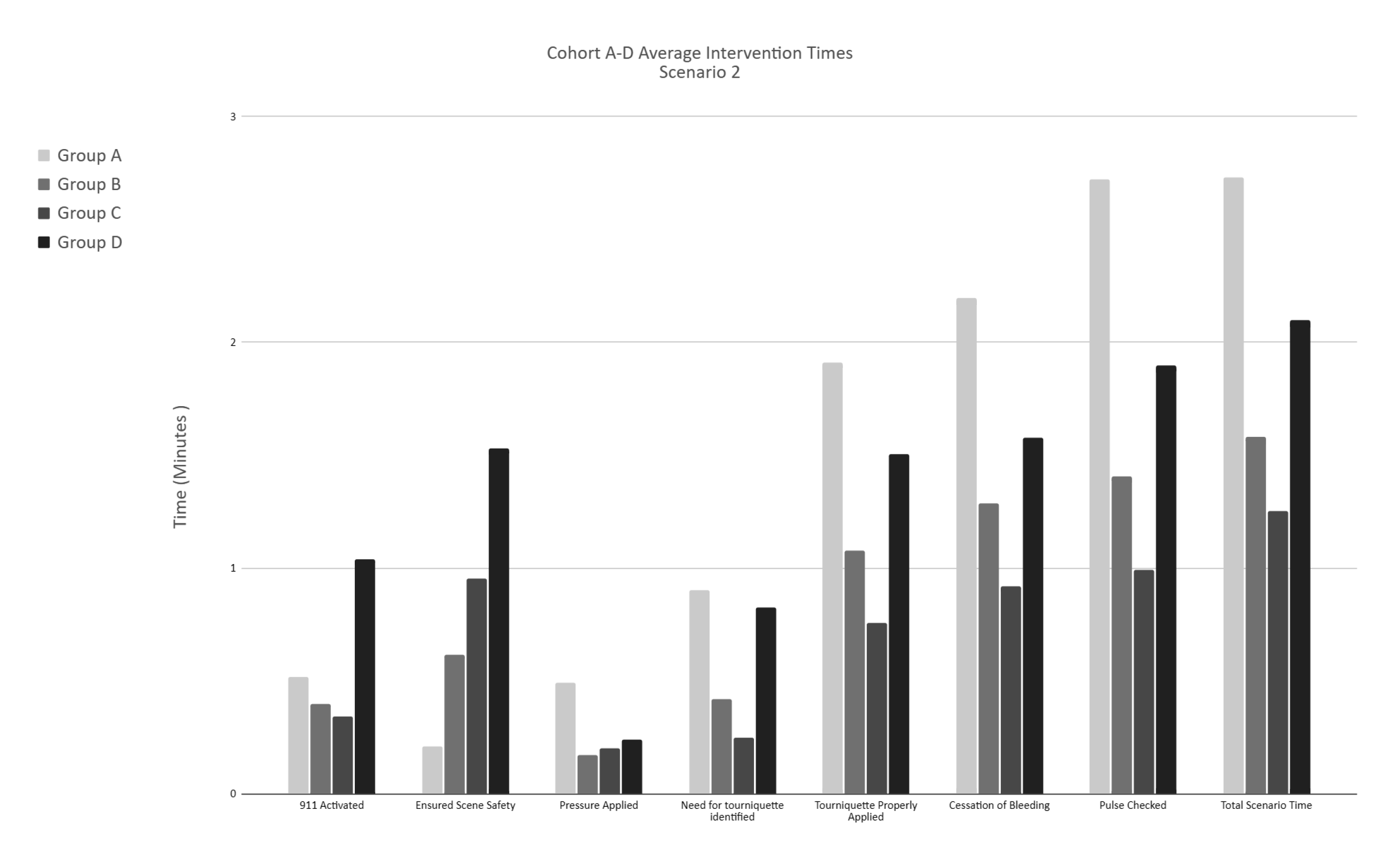 Cohort A-D Average Intervention Times, Scenario 2
Cohort A-D Average Intervention Times, Scenario 2Figure 1
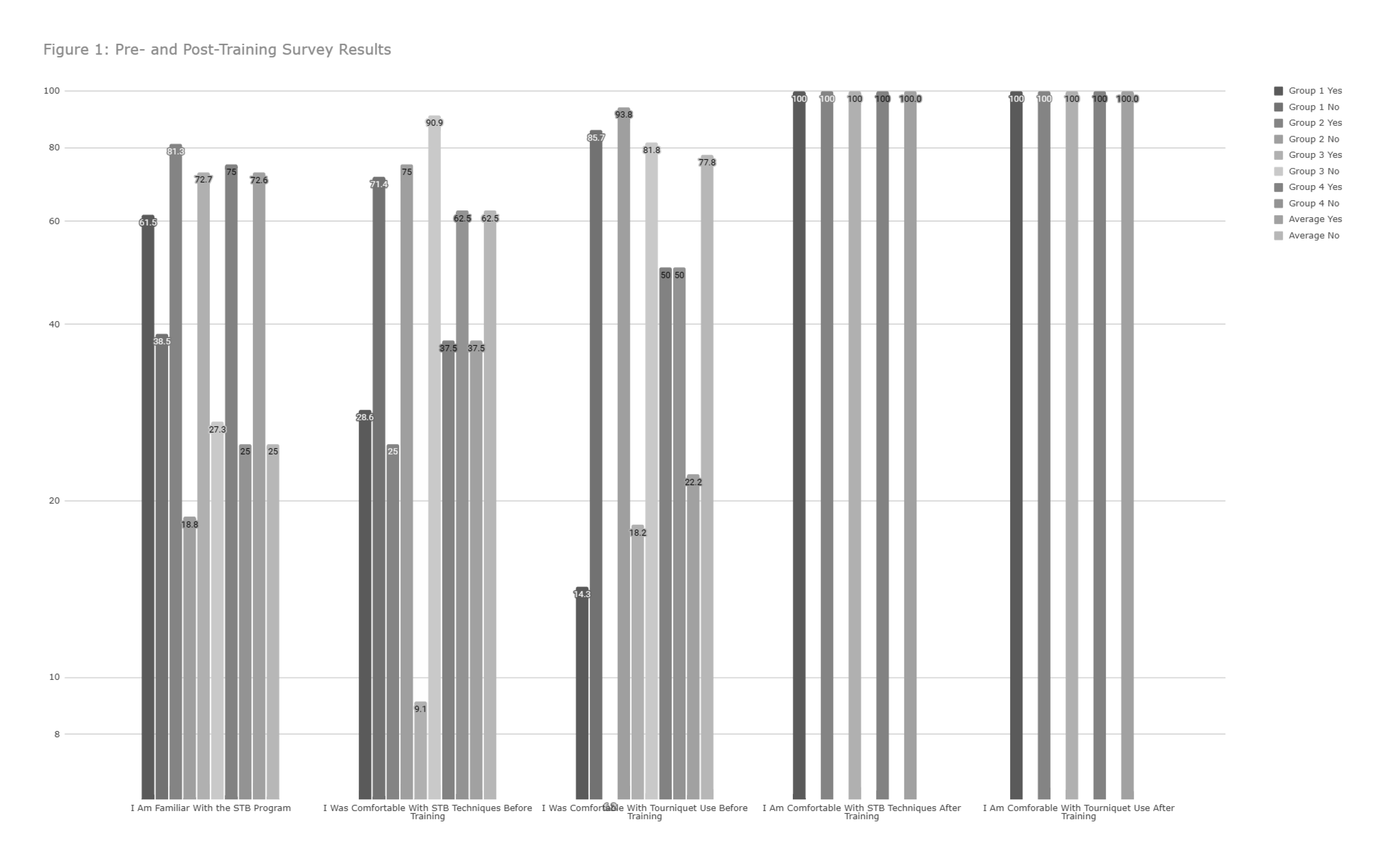 Pre- and Post-Training Survey Results
Pre- and Post-Training Survey Results Figure 2
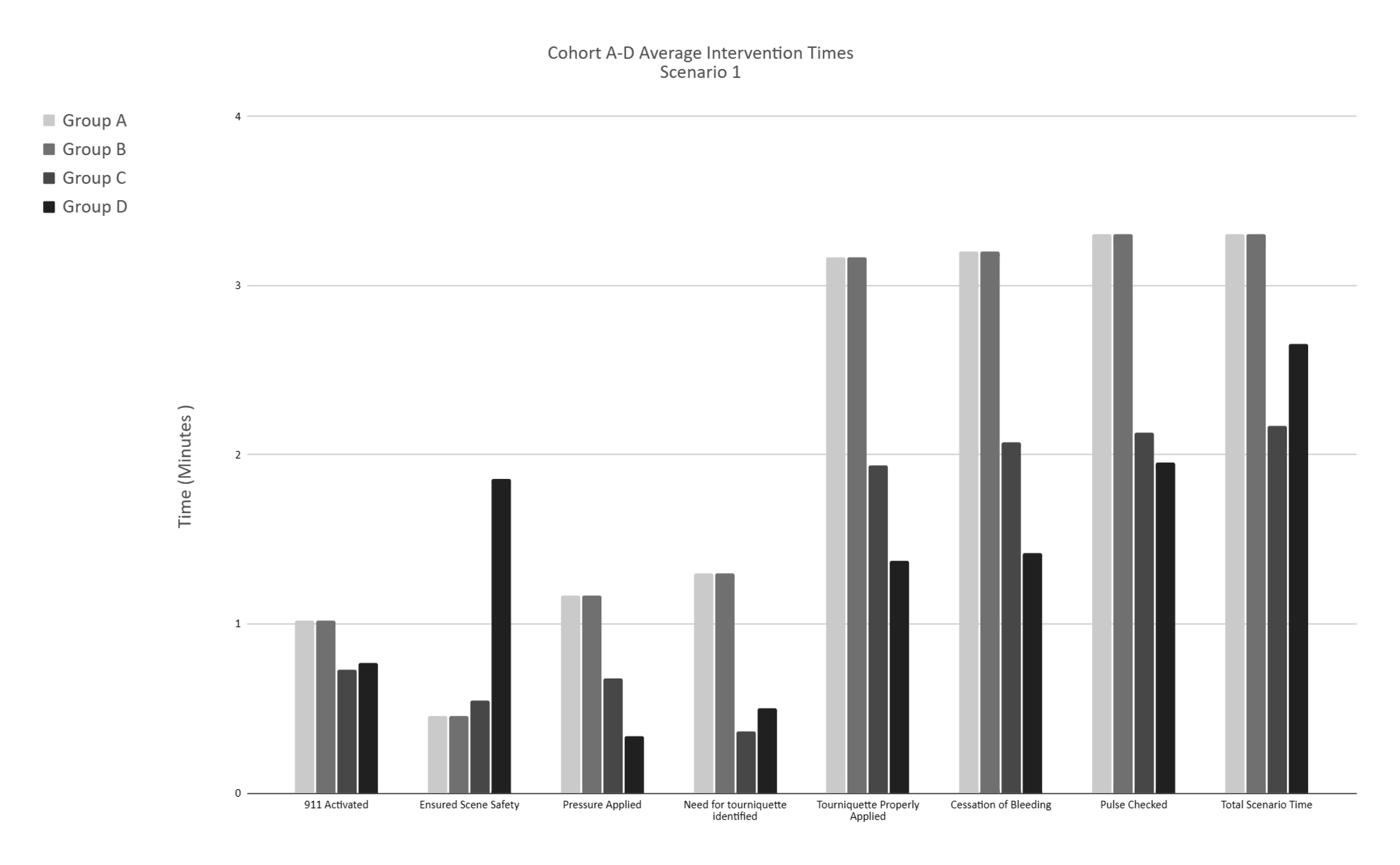 Cohort A-D Average Intervention Times, Scenario 1
Cohort A-D Average Intervention Times, Scenario 1Figure 3
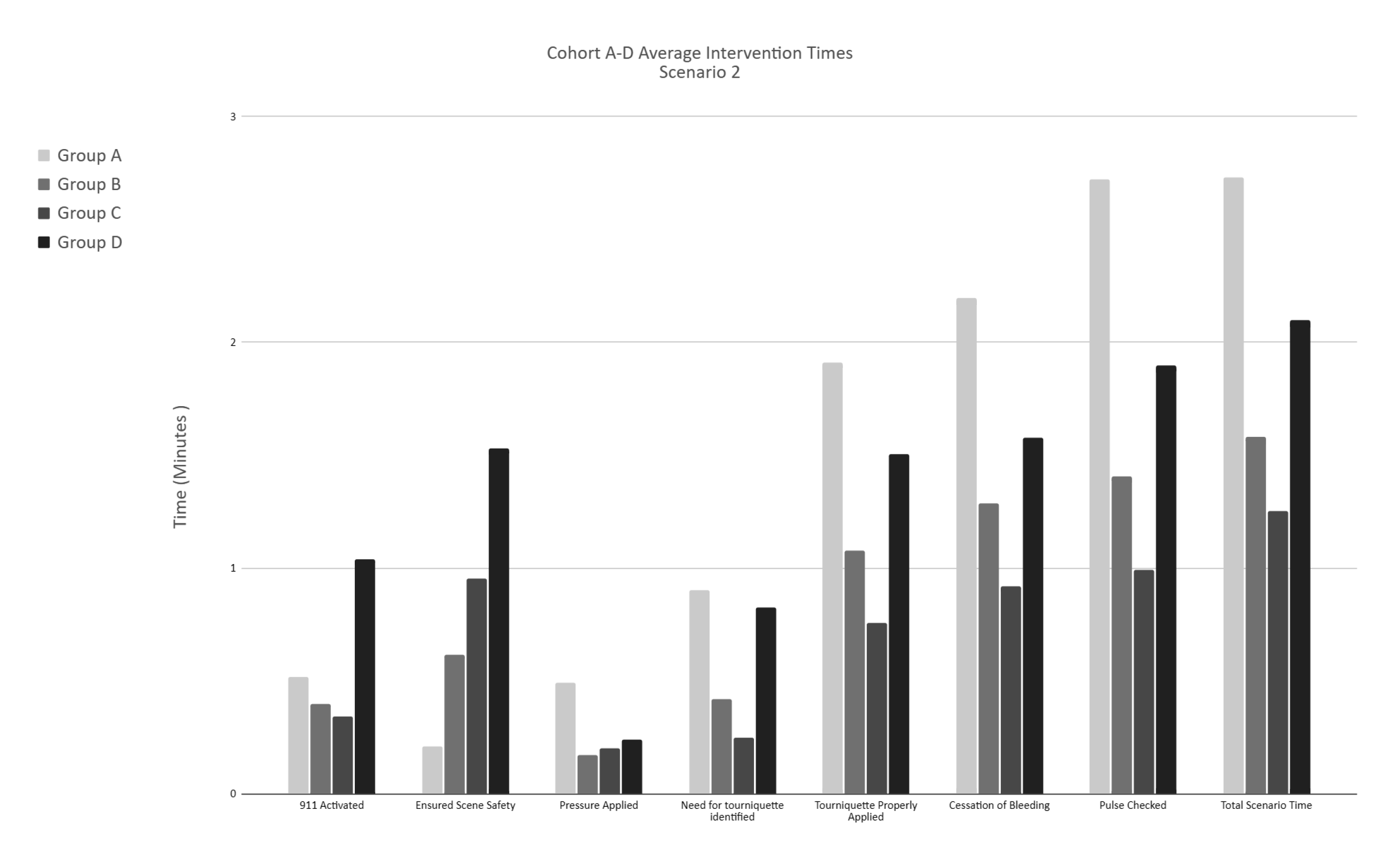 Cohort A-D Average Intervention Times, Scenario 2
Cohort A-D Average Intervention Times, Scenario 2
