Neonatal Quality Improvement 5
Session: Neonatal Quality Improvement 5
521 - Premedication Use for Controlled Intubations: A Quality Improvement Effort in a Level IV Neonatal Intensive Care Unit
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 521.6137
- NP
Nicholas Puoplo, MD (he/him/his)
NICU Fellow
New York Presbyterian- Columbia
Icahn School of Medicine at Mount Sinai Department of Pediatrics
Bronx, New York, United States
Presenting Author(s)
Background: Despite national recommendations to administer premedication prior to nonemergent intubations in the NICU, variability in adopting these practices exists despite benefits of premedication including decreased intubation attempts and improved long-term outcomes. Our level IV NICU composed of a 58-bed general NICU and 17-bed infant cardiac NICU, which performs 250 intubations a year, did not have formalized guidelines surrounding their usage representing an area for improvement.
Objective: To standardize a premedication regimen prior to controlled intubations including atropine and fentanyl, with rocuronium used in select cases. Secondarily, with increased premedication use we aimed to improve first-time intubation success rates.
Design/Methods: QI methodology including Plan-Do-Study-Act (PDSA) cycles was used to achieve our SMART aim within 1.5 years which was to increase premedication use from a baseline of 24% to 100% in neonates ≥23 weeks gestation who required controlled intubation and increase first attempt intubation success from 50% without premedication to 60%. Our multidisciplinary team included attending neonatologists, NICU fellows, pharmacists, nurses, nurse practitioners and respiratory therapists. Main PDSA cycles included creation and release of premedication guidelines, creation of an electronic order-set, education of all key stakeholders and standardizing tracking of adverse events. Our data was tracked in terms of atropine and fentanyl usage and intubation attempts. Our balancing measures included any intubation-related adverse events.
Results: The percentage of controlled intubations performed with atropine and fentanyl increased from our 6-month baseline of 24% to 78% within 1.5 years, notably with an early positive trend near guideline release followed by a positive shift after further education to the infant cardiac NICU as seen by the non-random patterns of our p-chart. Intubation success rates on first attempt decreased from 50% without premedication to 46% with premedication. There was no report of any premedication-related adverse event requiring a reversal agent (e.g. naloxone).
Conclusion(s): Premedication use prior to controlled intubations increased over an 18-month period following implementation of guidelines and interventions primarily aimed at education. Although first time intubation success rates did not improve, we implemented a set of standardized guidelines that match national standards, defining controlled intubation and adverse events. The next step includes increasing use of rocuronium with the current regimen, which has already begun in our unit.
Key Driver Diagram
.png) Key driver diagram created by multidisciplinary team that identifies the most important interventions necessary to influence our key drivers in order to reach our smart aim.
Key driver diagram created by multidisciplinary team that identifies the most important interventions necessary to influence our key drivers in order to reach our smart aim. Premedication for Controlled Intubation Algorithm
.png) Algorithm created to determine which intubations qualify as “controlled” and how to proceed on a patient-by-patient basis. QR code is included for intubation and adverse event tracking. This algorithm can be followed for every neonatal intubation.
Algorithm created to determine which intubations qualify as “controlled” and how to proceed on a patient-by-patient basis. QR code is included for intubation and adverse event tracking. This algorithm can be followed for every neonatal intubation.pChart Analysis of % Compliance in Atropine/Fentanyl Use in Controlled Intubations
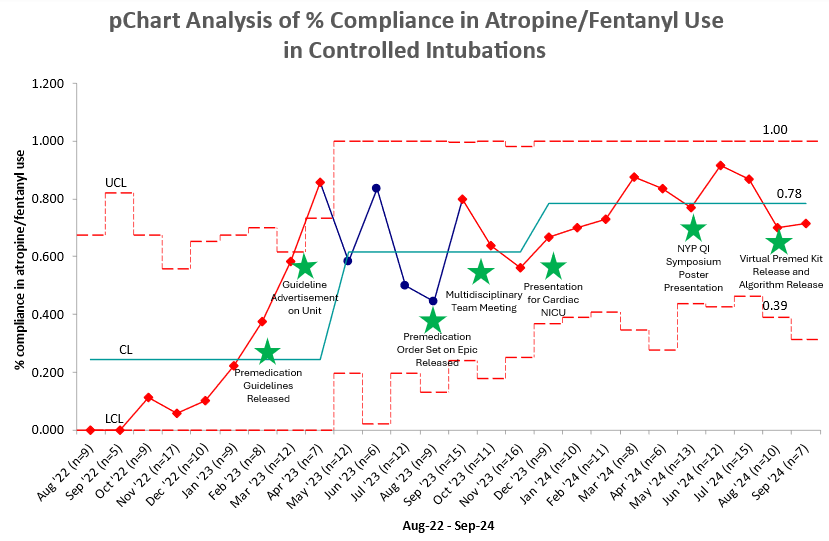 pChart showing monthly % compliance from August 2022 to September 2024 with PDSA cycles noted by stars. An early positive trend is noted from November 2022 to April 2023. A shift that changed our median was noted from December 2023 to July 2024.
pChart showing monthly % compliance from August 2022 to September 2024 with PDSA cycles noted by stars. An early positive trend is noted from November 2022 to April 2023. A shift that changed our median was noted from December 2023 to July 2024.Key Driver Diagram
.png) Key driver diagram created by multidisciplinary team that identifies the most important interventions necessary to influence our key drivers in order to reach our smart aim.
Key driver diagram created by multidisciplinary team that identifies the most important interventions necessary to influence our key drivers in order to reach our smart aim. Premedication for Controlled Intubation Algorithm
.png) Algorithm created to determine which intubations qualify as “controlled” and how to proceed on a patient-by-patient basis. QR code is included for intubation and adverse event tracking. This algorithm can be followed for every neonatal intubation.
Algorithm created to determine which intubations qualify as “controlled” and how to proceed on a patient-by-patient basis. QR code is included for intubation and adverse event tracking. This algorithm can be followed for every neonatal intubation.pChart Analysis of % Compliance in Atropine/Fentanyl Use in Controlled Intubations
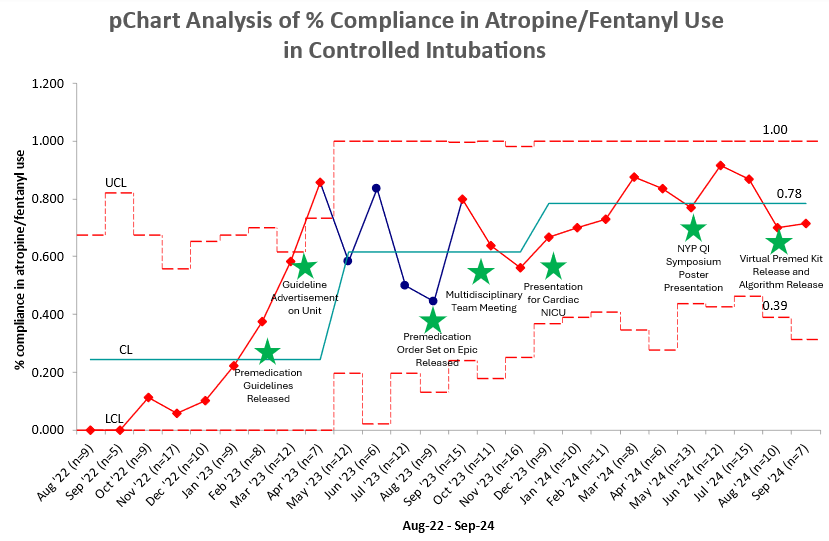 pChart showing monthly % compliance from August 2022 to September 2024 with PDSA cycles noted by stars. An early positive trend is noted from November 2022 to April 2023. A shift that changed our median was noted from December 2023 to July 2024.
pChart showing monthly % compliance from August 2022 to September 2024 with PDSA cycles noted by stars. An early positive trend is noted from November 2022 to April 2023. A shift that changed our median was noted from December 2023 to July 2024.

