Hematology/Oncology 1: Pediatric Oncology
Session: Hematology/Oncology 1: Pediatric Oncology
103 - Preferred Language, Acuity at Presentation, and Intensive Care Unit (ICU) Level Care in Children with Acute Myeloid Leukemia
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 103.6179
Jenny Ruiz, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Catherine Aftandilian, Stanford University School of Medicine, Palo Alto, CA, United States; Yimei Li, University of Pennsylvania, Philadelphia, PA, United States; Yuan-Shung Huang, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Caitlin W. Elgarten, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Regina Myers, The Children's Hospital of Philadelphia, Swarthmore, PA, United States; Daniel Zheng, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Haley Newman, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Tamara P.. Miller, Emory University School of Medicine, Atlanta, GA, United States; Kira Bona, Dana-Farber Cancer Institute/Boston Children's Hospital, Boston, MA, United States; Maria Monica Gramatges, Baylor College of Medicine, Houston, TX, United States; Taumoha Ghosh, Primary Children's Hospital, Salt Lake City, UT, United States; Kelly Maloney, Children's Hospital Colorado, Aurora, CO, United States; Arunkumar Modi, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Elaine R. morgan, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Naomi Winick, University of Texas Health Science Center, Dallas, TX, United States; Caroline Smith, University of Texas Southwestern Medical School, Dallas, TX, United States; Jennifer Wilkes, University of Washington School of Medicine, seattle, WA, United States; Brian Fisher, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Kelly D. Getz, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Richard Aplenc, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Alix Seif, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Jenny Ruiz, MD, MSCE (she/her/hers)
Assistant Professor of Pediatrics
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Racial and ethnic disparities in pediatric cancer outcomes persist despite treatment advancements. Social drivers of health, including language, are associated with pediatric adverse events, and may be intervenable. Few studies have examined language and outcomes in cancer with mixed results. Preferring languages other than English (LOE) may hinder effective communication with medical teams which may have downstream effects on outcomes. No studies have examined language and pediatric acute myeloid leukemia (AML) morbidity.
Objective: To examine the association between preferred language, high acuity, and ICU-level care in children with AML.
Design/Methods: We performed a secondary data analysis from a multi-institution, prospective cohort merged with daily resource utilization data from the Pediatric Health Information System database of AML patients treated between January 2011 to October 2023. Preferred language and other demographics were obtained from the electronic medical record per institutional standards and dichotomized as LOE vs English (reference). Outcomes included high acuity (≥2 organ systems requiring ICU-level care during the first 72-hours of initial admission) and any ICU-level care during the first cycle. Covariates (age, sex, ethnicity, race, insurance, year of diagnosis, risk classification, and trial enrollment) were compared by language. Unadjusted and adjusted logistic or log binomial regression models were performed. We used a directed acyclic graph (DAG) to select confounders (age, sex, income, race-ethnicity) a priori to include in our adjusted models. Race-ethnicity was highly collinear with language and thus not included in the final model.
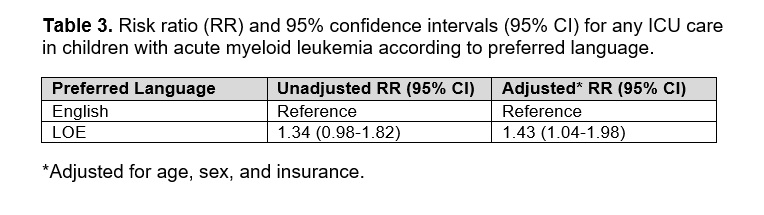
Results: 490 patients were identified from 8 institutions and 56 (11%) preferred LOE. Spanish was the most common (91%) LOE. Patients who preferred LOE were more likely to be male (68%), Hispanic (89%), have public insurance or be uninsured vs private insurance (95%) (Table 1). The mean inpatient days in the first cycle was 40; this did not differ by language. In adjusted analyses, LOE was associated with high acuity (14% vs 8%; aOR=2.32, 95% CI 0.92-5.38) and this approached significance (Table 2). In adjusted analyses, LOE was associated with any ICU care (46% vs 35%; aRR=1.43, 95% Cl 1.04-1.98) (Table 3).
Conclusion(s): AML patients with preferred LOE have greater than 2 times higher odds of high acuity at presentation compared to patients who prefer English and have significantly greater risk of requiring ICU-level care in the first cycle. These findings support the need to investigate the role language plays in cancer treatment.
Table 1. Socio-demographics of patients by preferred language.
.jpg)
Table 2. Odds ratio (OR) and 95% confidence intervals (95% CI) for high acuity in children with acute myeloid leukemia according to preferred language.
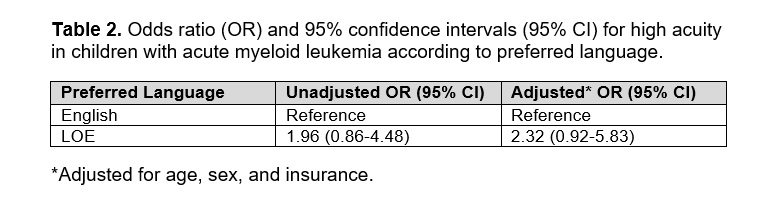
Table 3. Risk ratio (RR) and 95% confidence intervals (95% CI) for any ICU care in children with acute myeloid leukemia according to preferred language.