Quality Improvement/Patient Safety 5
Session: Quality Improvement/Patient Safety 5
479 - Quality Improvement Initiative to Increase Resident Safety Event Reporting in the Pediatric Department
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 479.6255
Matthew J. Tam, NewYork-Presbyterian Komansky Children’s Hospital, New York City, NY, United States; Caitlin Ehret, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Erika Abramson, Weill Cornell Medicine, Rye Brook, NY, United States; Snezana Osorio, Weill Cornell Medicine, New York, NY, United States

Matthew J. Tam, MD (he/him/his)
Resident
NewYork-Presbyterian Komansky Children’s Hospital
New York City, New York, United States
Presenting Author(s)
Background: The American Academy of Pediatrics (AAP) has recognized the importance of safety event reporting in minimizing adverse events, near misses, and unsafe conditions. Despite this, resident-submitted events represent a small fraction of total safety events in hospital systems. Studies have demonstrated that key barriers to resident reporting include resident perception of inadequate system change, inadequate feedback, time to submit, and failure to identify the appropriateness of events to report.
Objective: To increase the rate of resident-reported safety concerns from 1.29% to 10% by June 28th, 2025.
Design/Methods: This is an observational study with planned sequential experimentation at a tertiary academic medical center. A resident-led team, which included attending physicians and a patient safety specialist, designed the Key Driver Diagram (Figure 1). Change ideas have been implemented via 3 PDSA cycles including education, monthly meetings, a newsletter, reporting system improvement, shadowing of event reviews, and incoming-PGY1 teachings (Figure 2). Data was extracted through the campus-wide self-reporting system for all pediatric care locations. The outcome measure was the rate of safety concerns submitted by pediatric residents. The process measures included timely and completed reports defined as reports submitted within 48 hours of an event, with the inclusion of setting, involved parties, and a summarized description. The balancing measure was resident self-reported time required to submit a safety concern. We used statistical process “P” charts to display and analyze data. We applied API rules to detect special cause variation.
Results: In this sample of 58 resident-reported safety concerns, the rate of reporting improved from a baseline of 1.29% to 7.55% (Figure 2). Total of 56 submitted reports were considered timely and fully completed as defined by our process measure definitions (Figure 3). The average self-reported time to submit a safety concern remained stable at 14 minutes (balancing measure).
Conclusion(s): Enhancing pediatric resident safety concern event reporting requires a multifaceted approach that addresses educational, procedural, and cultural factors. Our interventions have demonstrated special cause variation in the reporting rate of non-anonymous pediatric resident safety event reporting. Future PDSA intervention steps include sharing completed event review content with resident reporters and further enhancement of the reporting tool to facilitate resident event reporting.
Figure 1
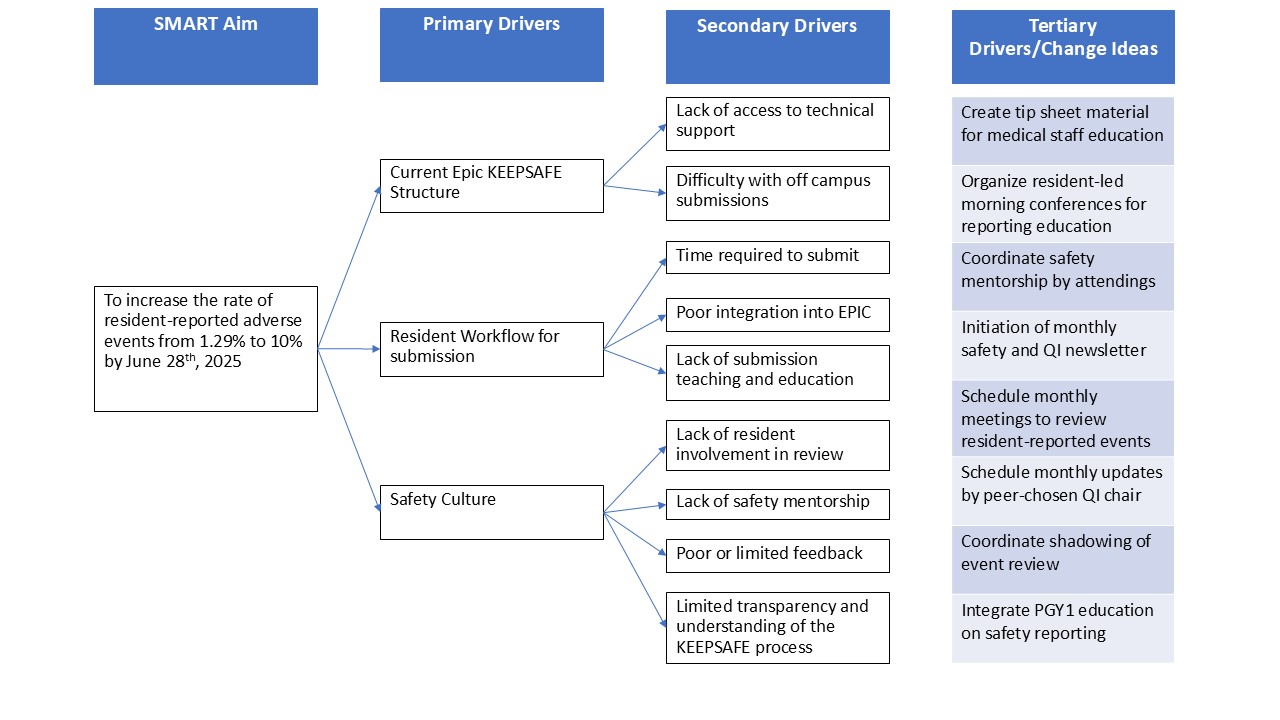 Key Driver Diagram
Key Driver DiagramFigure 2
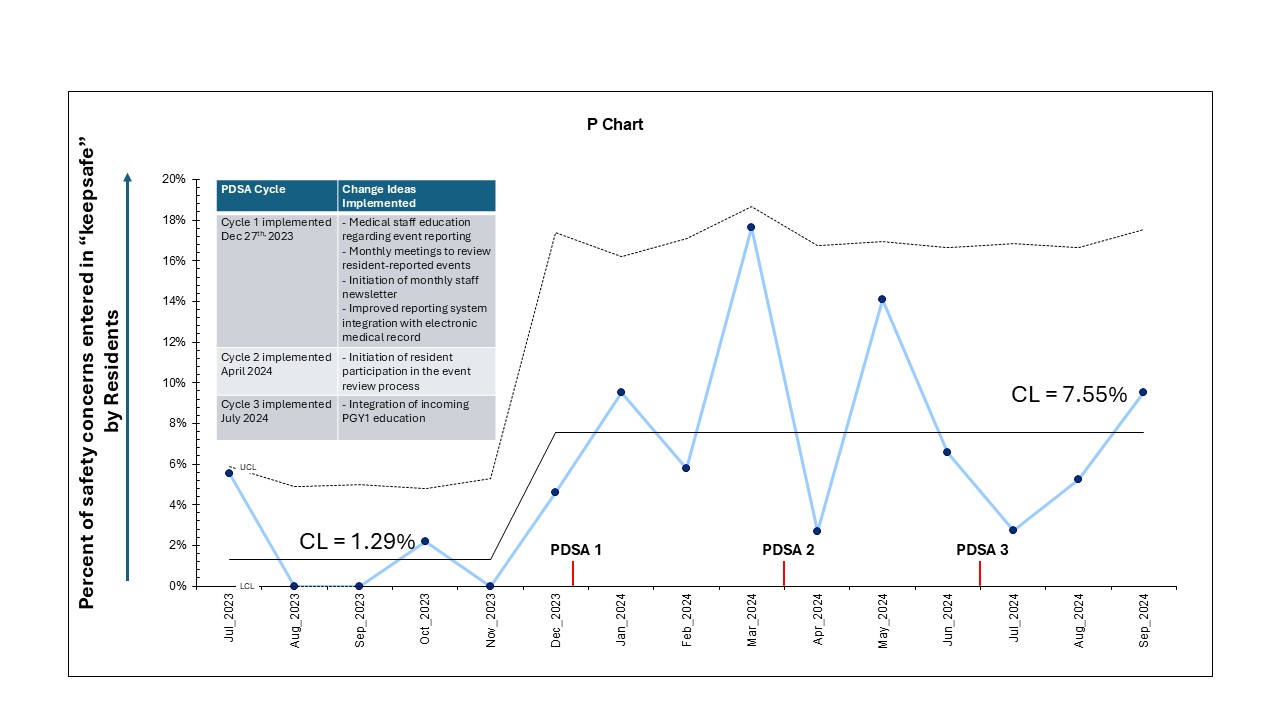 Pediatric residents' safety concern event reporting increased from 1.29% to 7.55%
Pediatric residents' safety concern event reporting increased from 1.29% to 7.55%Figure 3
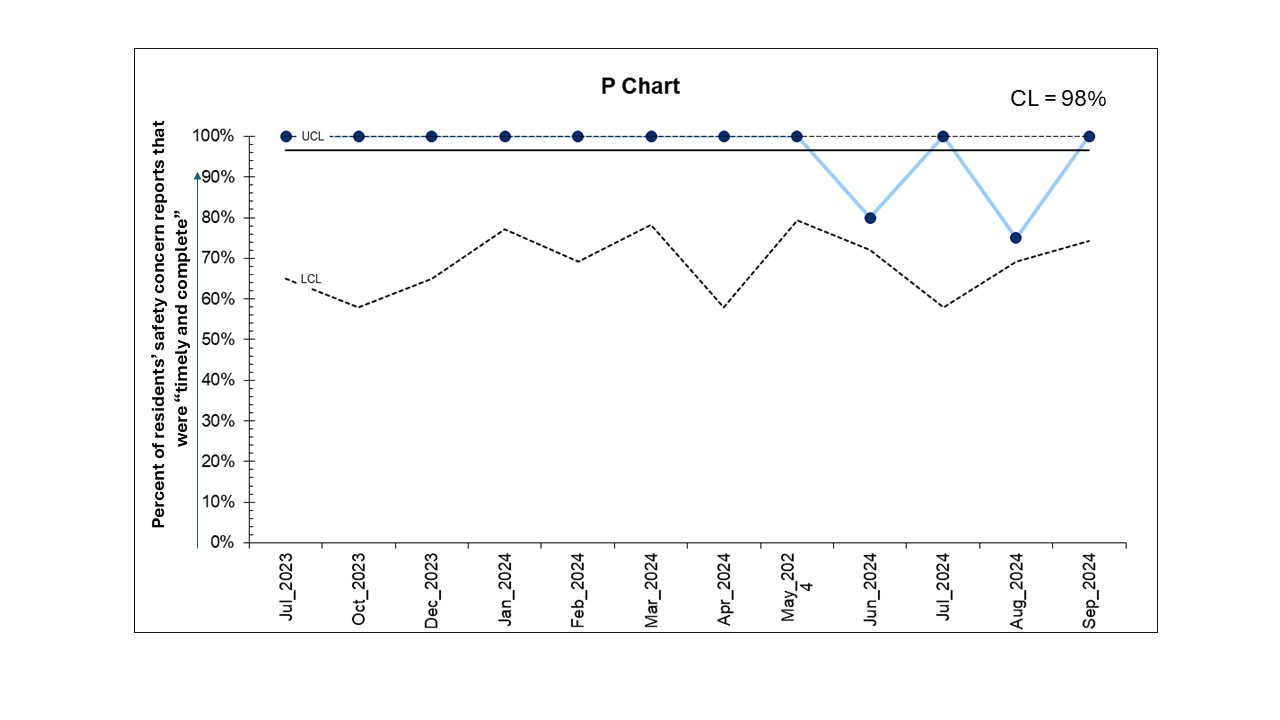 Safety Concern Reports: Resident provided all requested information within 48 hours following an event
Safety Concern Reports: Resident provided all requested information within 48 hours following an event

