Clinical Bioethics
Session: Clinical Bioethics
584 - Provider Perceptions of End-of-Life Care Decision Making in the NICU and PICU
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 584.6259
Nithya Sivakumar, University of California, Davis, School of Medicine, Sacramento, CA, United States; Stephanie K.. Kukora, Children's Research Institute, Children's Mercy Hospital, Children's Mercy, Kansas City, MO, United States; Cherie Ginwalla, University of California, Davis, School of Medicine, Sacramento, CA, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States; Jennifer Rosenthal, University of California, Davis, School of Medicine, Sacramento, CA, United States
- NS
Nithya Sivakumar, BA, MBE (she/her/hers)
Medical Student
University of California, Davis, School of Medicine
Sacramento, California, United States
Presenting Author(s)
Background: Neonatal intensive care unit (NICU) patients are more likely to be removed from life sustaining interventions sooner and more often than their older counterparts in the pediatric intensive care unit (PICU). Decision-making around life sustaining interventions may differ between the NICU and PICU, and this difference may be influenced by providers’ perceptions of parental values.
Objective: To evaluate and compare NICU and PICU providers’ perceptions of values that families considered when making end-of-life care decisions for their child.
Design/Methods: This single-site cross-sectional study used a survey to collect NICU and PICU providers’ perceptions of what families valued during end-of-life care decisions; providers were asked to consider their last patient for whom end of life care was considered. The items of the preliminary survey were informed by review of existing literature and revised based on feedback from 9 content experts. The survey was then iteratively refined through 6 cognitive interviews with providers until no further issues were identified. The final survey was sent to NICU and PICU providers. Descriptive statistics, including t-tests, were used to analyze data.
Results: A total of 69 survey participants completed the survey, of which 40 and 29 were NICU and PICU providers, respectively (Table 1). Most PICU (52%) respondents reported that end-of-life care discussions occurred within the first weeks of hospitalization, whereas many NICU respondents (38%) reported that they occurred within the first days (Figure 2A). Responses between NICU and PICU providers were similar across all other items (Table 2B, 2C, 2D). Providers in the NICU and PICU agreed that the family considered a range of factors, including likelihood of disability, quality of life, and religious/cultural beliefs, and valued factors such as finances and competing responsibilities less. Respondents also ranked the values that they perceived families prioritize (Table 3). There were no significant differences found between the values providers perceived to be important to families in the NICU and in the PICU.
Conclusion(s): Our survey did not identify differences in the values that providers in the NICU and PICU perceived to be important to families when making end-of-life care decisions. Further research in larger sample sizes and in multiple centers is warranted.
Table 1
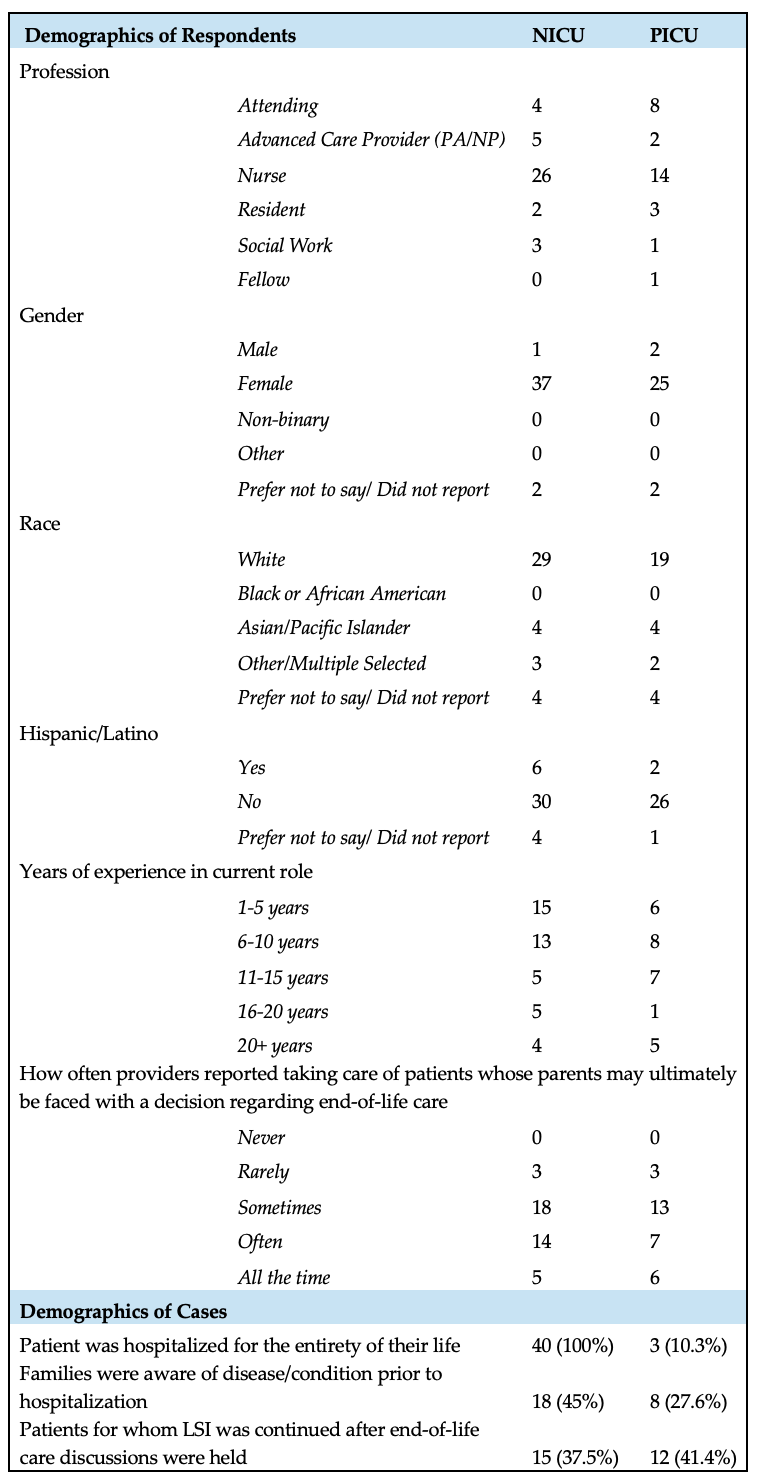 Demographic information for respondents and cases. There were 40 responses from providers in the NICU, and 29 from providers in the PICU.
Demographic information for respondents and cases. There were 40 responses from providers in the NICU, and 29 from providers in the PICU. Figure 1
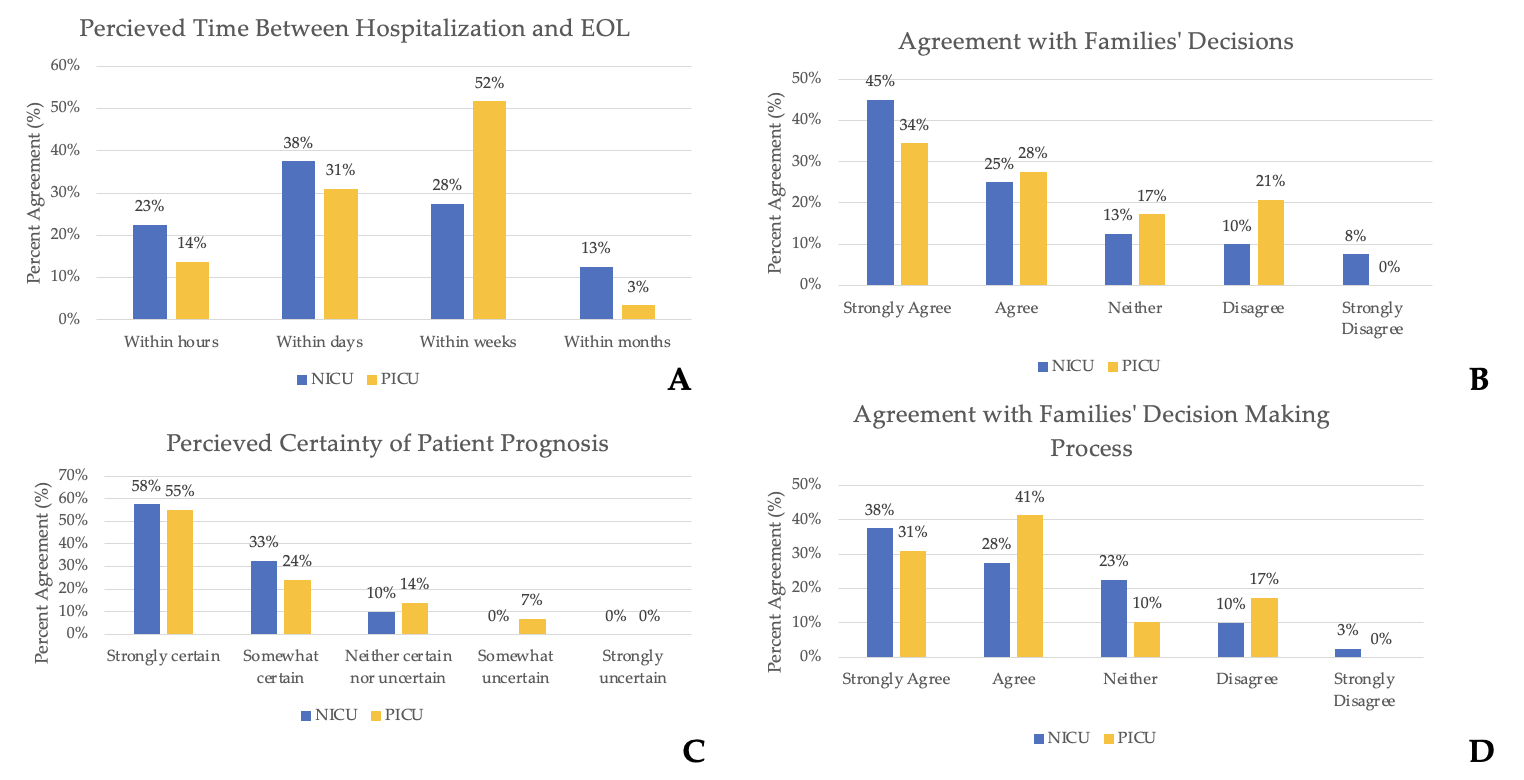 (A) Bar chart depicting perceived time between hospitalization and end of life (EOL) care discussions. (B) Bar chart depicting provider agreement with families’ decision regarding continuing or withdrawing life sustaining therapy after end-of-life care discussions. (C) Bar chart depicting perceived certainty of patient prognosis at the time of end-of-life care discussions. (D) Bar chart depicting provider agreement with how families came to the decision regarding whether to continue or withdraw life sustaining therapies after end-of-life care discussions.
(A) Bar chart depicting perceived time between hospitalization and end of life (EOL) care discussions. (B) Bar chart depicting provider agreement with families’ decision regarding continuing or withdrawing life sustaining therapy after end-of-life care discussions. (C) Bar chart depicting perceived certainty of patient prognosis at the time of end-of-life care discussions. (D) Bar chart depicting provider agreement with how families came to the decision regarding whether to continue or withdraw life sustaining therapies after end-of-life care discussions.Table 2
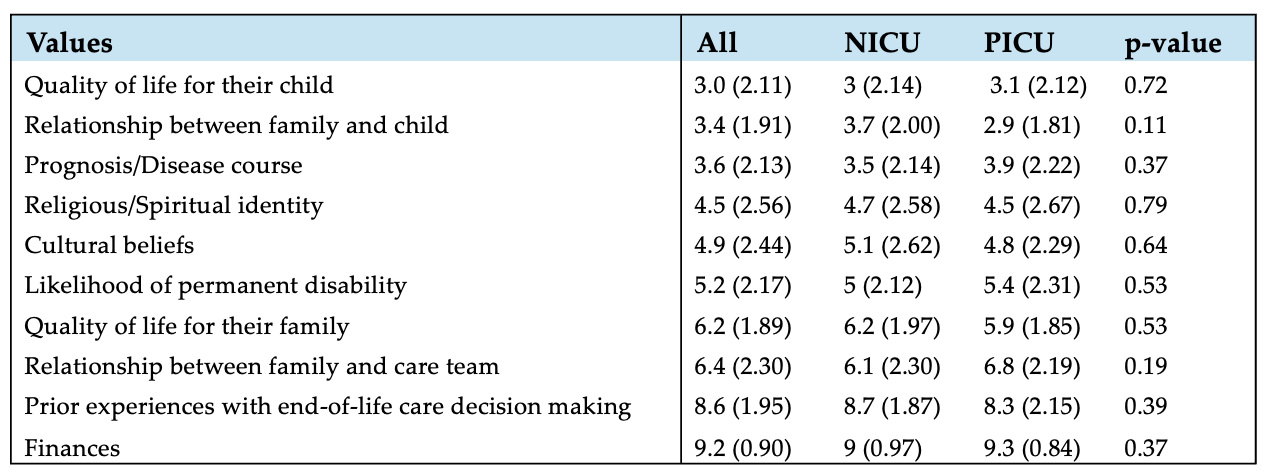 Results on ranking question of the research survey. Respondents were asked to rank values that their family considered from most (1) to least (10) important, reported as mean (standard deviation).
Results on ranking question of the research survey. Respondents were asked to rank values that their family considered from most (1) to least (10) important, reported as mean (standard deviation). 
