Neonatal Nephrology/AKI 1
Session: Neonatal Nephrology/AKI 1
013 - Renal Oxygenation Increases with Postmenstrual Age in Preterm Neonates
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 13.6226
Derek M. Gross, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Shayla Schwingle, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Cassandra E.. Nelson, UW Madison Dept of Pediatrics PCRC, Madison, WI, United States; Eli J. Cowan, University of Wisconsin School of Medicine and Public Health, Bellaire, TX, United States; Matthew W. Harer, University of Wisconsin School of Medicine and Public Health, Waunakee, WI, United States

Derek M. Gross (he/him/his)
Medical Studenntt
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background: Preterm neonates born < 32 weeks gestational age (GA) have underdeveloped kidneys and are susceptible to acute kidney injury (AKI) in the neonatal intensive care unit (NICU). Near-infrared spectroscopy (NIRS) allows for non-invasive measurement of renal tissue oxygenation (RrSO₂) and provides a potential means for early detection of decreased renal perfusion. Studies in preterm neonates have shown normal RrSO₂ values between 50-80% within the first two weeks of life; however, there is limited knowledge of how RrSO₂ changes as neonates mature to term-corrected postmenstrual age (PMA).
Objective: We aimed to characterize developmental changes in RrSO₂ in preterm neonates based on PMA. We hypothesized that RrSO₂ would increase as PMA increased.
Design/Methods: Preterm neonates < 32 weeks GA were enrolled in a prospective observational NIRS monitoring study. Neonatal INVOS NIRS sensors were placed on the flanks of neonates and recorded RrSO₂ every 5 seconds for 3-4 hours each week until NICU discharge. For analysis, RrSO₂ measurements were converted to weekly mean RrSO₂ values. Median RrSO₂ values for each PMA were then calculated from each neonate’s weekly mean RrSO₂. We planned a subgroup analysis to compare extremely preterm (born < 28 weeks GA) and very preterm (28-31 6/7 weeks GA) neonates. Statistical analysis was performed with GraphPad Prism 9.
Results: Of 112 enrolled neonates, 100 neonates (56 male, 44 female) with a mean GA of 28.5 weeks (SD 2.2, range 23-32) and a mean birth weight of 1250 grams (SD 368, range 360-1980) received weekly renal NIRS monitoring. The mean RrSO₂ from 28 to 40 weeks PMA was 67.8% (SD 9.73). The distribution of RrSO₂ is displayed in Figure 1 and was different across PMA (p < 0.01; Kruskal-Wallis). There was also a positive correlation with median RrSO₂ and PMA (R2 = 0.63, p < 0.01; simple linear regression; Figure 2). Analysis by GA revealed extremely preterm neonates maintained a positive correlation between median RrSO₂ and PMA (R2 = 0.73, p < 0.01), but very preterm neonates did not (R2 = 0.039, p = 0.54; Figure 3).
Conclusion(s): This study demonstrates that RrSO₂ in preterm neonates increases in a linear fashion with advancing PMA, with the trend most pronounced in extremely preterm neonates. Increasing RrSO₂ with advancing PMA in extremely preterm neonates may reflect delayed renal maturation and vascular development that typically occurs in-utero. Very preterm neonates may have more stable RrSO₂ with advancing PMA due to more advanced in-utero kidney development or more rapid maturity in the initial weeks of life than extremely premature neonates.
Figure 1. RrSO₂ Across Postmenstrual Ages in Preterm Neonates <32 weeks GA
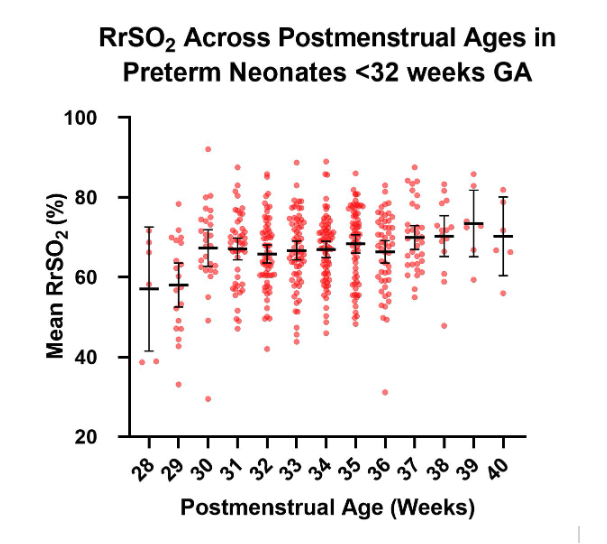 Scatter plot depicting mean RrSO₂ values by PMA. Individual data points represent mean RrSO₂ values for each neonate per PMA week. Shapiro-Wilk testing indicated that the data was not normally distributed; therefore, medians and interquartile ranges (IQR) are overlaid for each PMA to illustrate central tendency and variability in RrSO₂ among the 100 neonates.
Scatter plot depicting mean RrSO₂ values by PMA. Individual data points represent mean RrSO₂ values for each neonate per PMA week. Shapiro-Wilk testing indicated that the data was not normally distributed; therefore, medians and interquartile ranges (IQR) are overlaid for each PMA to illustrate central tendency and variability in RrSO₂ among the 100 neonates.Figure 2. RrSO₂ Increases with Postmenstrual Age in Preterm Neonates <32 weeks GA
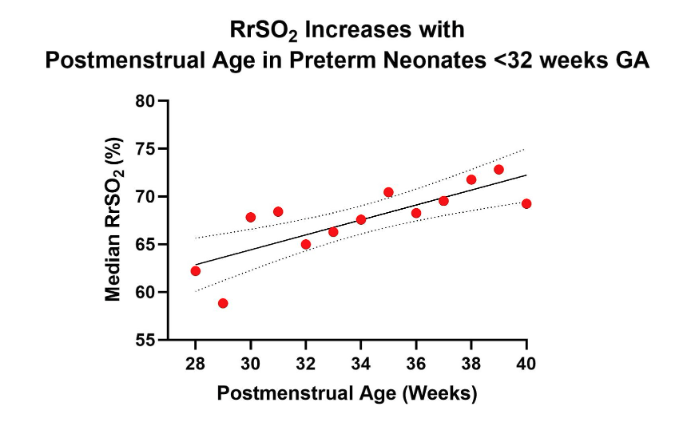 Simple linear regression plot showing the relationship between median RrSO₂ and PMA in weeks. Each data point represents the median RrSO₂ for a given PMA week. There was a positive correlation between median RrSO₂ and PMA (R2 = 0.63, p < 0.01).
Simple linear regression plot showing the relationship between median RrSO₂ and PMA in weeks. Each data point represents the median RrSO₂ for a given PMA week. There was a positive correlation between median RrSO₂ and PMA (R2 = 0.63, p < 0.01).Figure 3. Gestational Age Differences in RrSO₂ Across Postmenstrual Ages.
.png) Line graph depicting the median RrSO₂ for each PMA in two gestational age (GA) groups, extremely preterm (n = 28) and very preterm (n = 72). There was a positive correlation between RrSO₂ and PMA in the extremely preterm group (R2 = 0.73, p < 0.01; simple linear regression), while the very preterm group did not have a significant correlation (R2 = 0.039 p = 0.54).
Line graph depicting the median RrSO₂ for each PMA in two gestational age (GA) groups, extremely preterm (n = 28) and very preterm (n = 72). There was a positive correlation between RrSO₂ and PMA in the extremely preterm group (R2 = 0.73, p < 0.01; simple linear regression), while the very preterm group did not have a significant correlation (R2 = 0.039 p = 0.54).
