Neonatal Quality Improvement 5
Session: Neonatal Quality Improvement 5
527 - Triglyceride Monitoring in VLBW Infants: A Quality Improvement Initiative
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 527.6701
Ernest Lai, University of California, Irvine, School of Medicine, Santa Ana, CA, United States; Robin M. Koeppel, University of California, Irvine, School of Medicine, Yorba Linda, CA, United States; Lisa Perumean, UCI Health, Orange, CA, United States; Yona Nicolau, University of California, Irvine, School of Medicine, Orange, CA, United States

Ernest Lai, MD
Neonatology Fellow
CHOC Children's Hospital of Orange County / University of California, Irvine, School of Medicine
Santa Ana, California, United States
Presenting Author(s)
Background: Preterm infants are at increased risk for hypertriglyceridemia (HTG) due to their physiologic immaturity and dependence on intravenous lipid emulsions (ILE) as a source of essential fatty acids and calories while on parenteral nutrition. Infants with birth weight (BW) below 1000 grams and gestational age under 28 weeks are at the greatest risk for HTG. However, within our institution and across others, practices for triglyceride monitoring vary, and there is no established consensus on the timing or criteria for HTG screening. A review of baseline data at our institution indicates potential over-screening for HTG.
Objective: To reduce the number of blood draws for triglyceride level (TGL) monitoring by 20% in infants with BW ≤ 1500g within the first month of life over 12-months.
Design/Methods: A retrospective chart review of 189 preterm infants with BW ≤ 1500g admitted from 2020 to 2022 revealed an incidence of HTG (>300 mg/dL) of 13.6%. Among those with HTG, fewer than 10% had BW > 1000g, with an overall HTG incidence of < 2% in this subset. Additional analysis identified inconsistencies in the ILE dose (g/kg) at which initial TGL were checked as ILE doses were increased. Based on these findings, new triglyceride screening guidelines were implemented in December 2023, recommending TGL testing only in infants with BW ≤ 1000g, unless medically indicated (e.g., septic shock, perinatal depression, persistent hyperglycemia). The guidelines also standardized the first TGL check to occur at an ILE dose of 3g/kg. The primary outcome measure is the number of TGL tests per 1000 total parenteral nutrition (TPN) days in the first month of life, with a secondary outcome of TGL tests per 1000 TPN days in the subset with BW > 1000g. Process measures include guideline compliance monitored through electronic medical record audits, while balancing measures include the frequency of severe HTG (>500 mg/dL). Statistical process control charts will track these measures, with updates after each PDSA cycle. Preliminary findings were presented as a Work in Progress abstract at PAS 2024.
Results: Among all infants with BW ≤ 1500g, there has been a 46.5% decrease in TGL tests per 1000 TPN days (Figure 1). In the subgroup with BW > 1000g, TGL tests per 1000 TPN days have decreased by 76% (Figure 2). Protocol adherence has averaged 83%, with no increase in severe HTG events (Figure 3).
Conclusion(s): Within 12 months, we successfully achieved a reduction of more than 20% in the number of TGL tests per 1000 TPN days during the first month of life in infants with BW ≤ 1500g, without an increase in the frequency of severe HTG events.
Figure 1
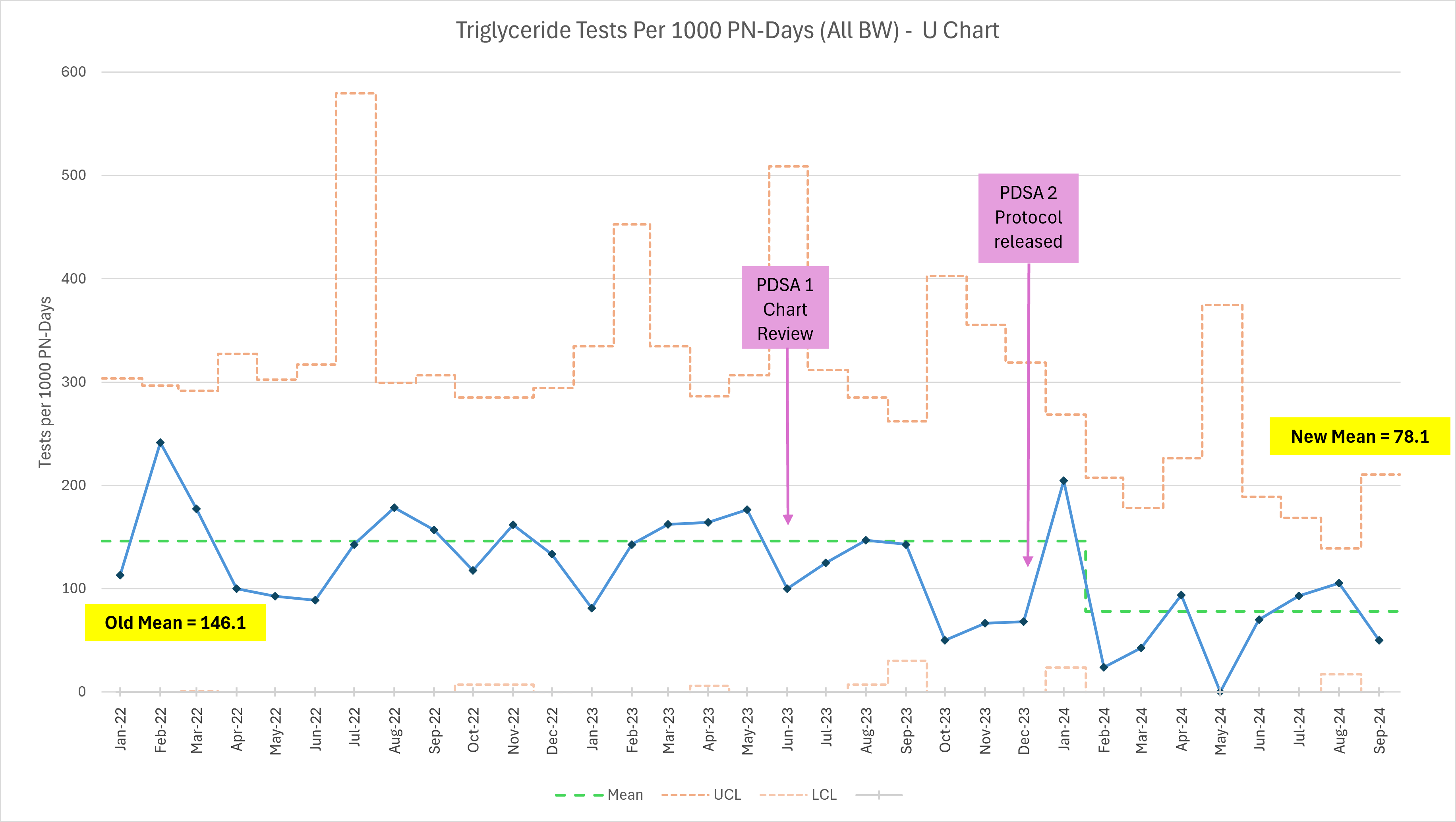 Primary outcome measure – annotated U chart depicting the number of triglyceride tests per 1000 parental nutrition days by month in all infants with BW ≤ 1500g from January 2022 through September 2024. UCL, upper control limit; LCL, lower control limit.
Primary outcome measure – annotated U chart depicting the number of triglyceride tests per 1000 parental nutrition days by month in all infants with BW ≤ 1500g from January 2022 through September 2024. UCL, upper control limit; LCL, lower control limit.Figure 2
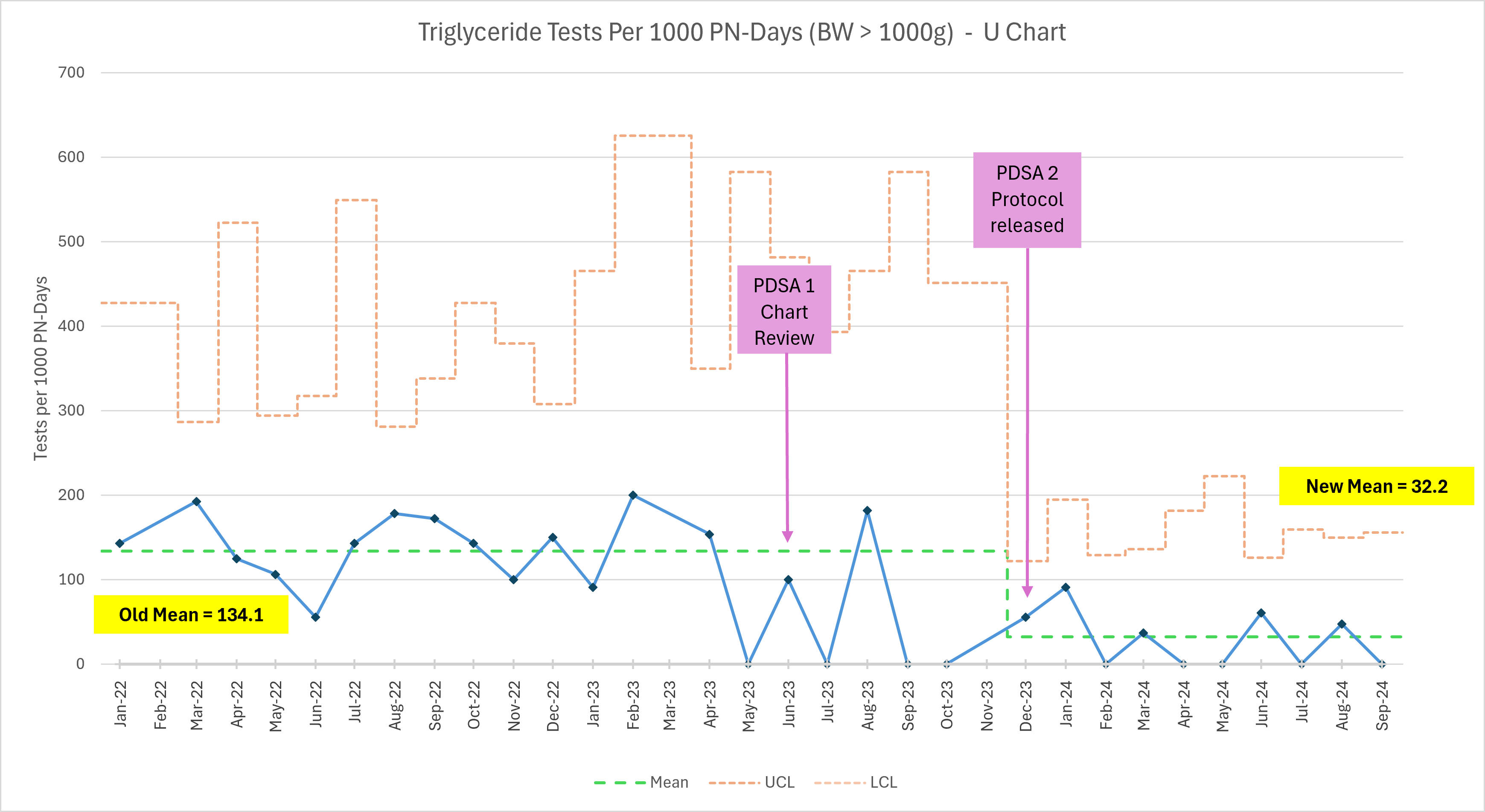 Secondary outcome measure – annotated U chart depicting the number of triglyceride tests per 1000 parental nutrition days by month in infants with BW > 1000g from January 2022 through September 2024. UCL, upper control limit; LCL, lower control limit.
Secondary outcome measure – annotated U chart depicting the number of triglyceride tests per 1000 parental nutrition days by month in infants with BW > 1000g from January 2022 through September 2024. UCL, upper control limit; LCL, lower control limit.Figure 3
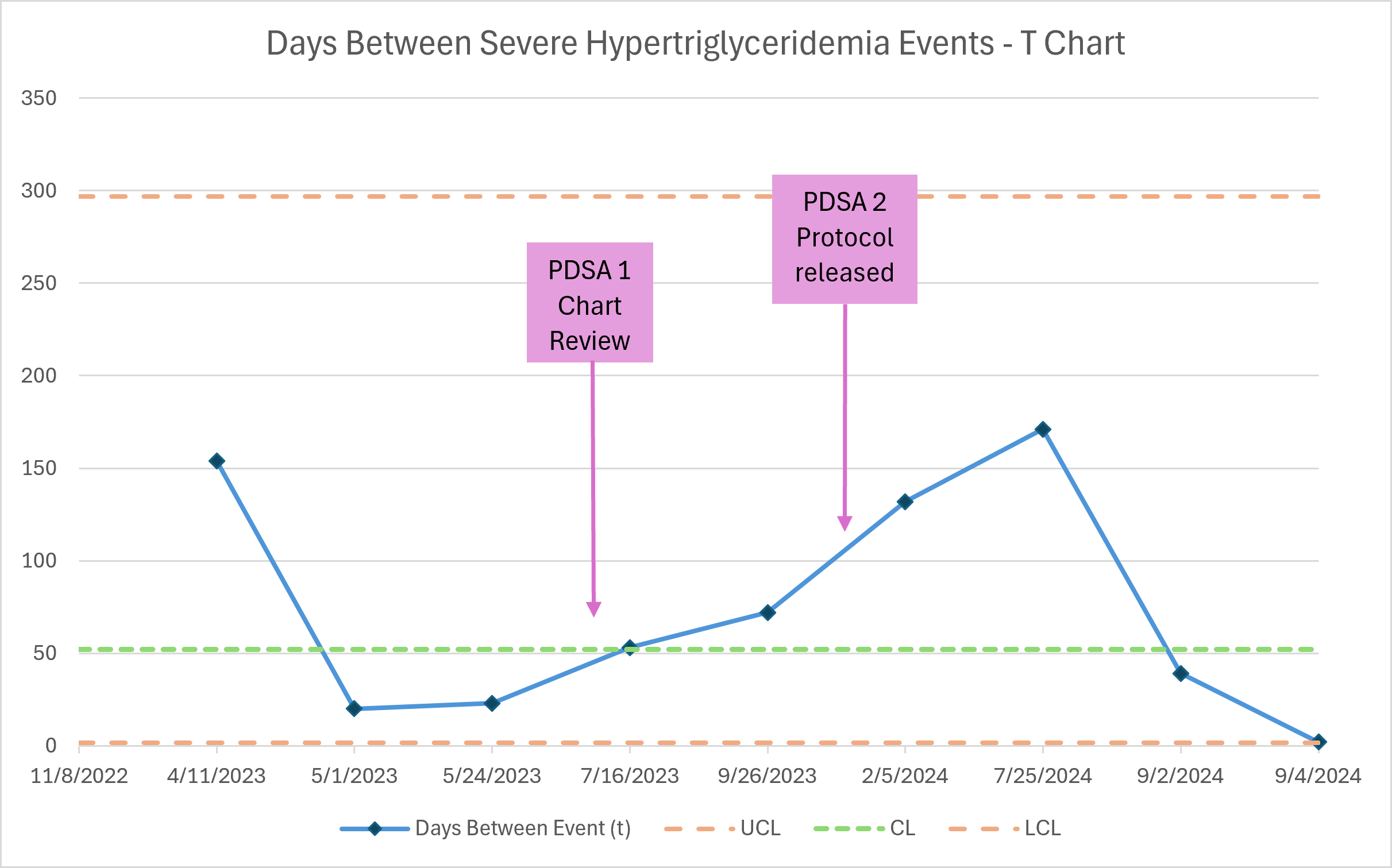 Balancing measure – annotated T chart depicting days between severe hypertriglyceridemia events (defined as a serum TG > 500 mg/dL) in all infants with BW ≤ 1500g from January 2022 through September 2024. UCL, upper control limit; LCL, lower control limit; CL, center line.
Balancing measure – annotated T chart depicting days between severe hypertriglyceridemia events (defined as a serum TG > 500 mg/dL) in all infants with BW ≤ 1500g from January 2022 through September 2024. UCL, upper control limit; LCL, lower control limit; CL, center line. 
