Emergency Medicine 6
Session: Emergency Medicine 6
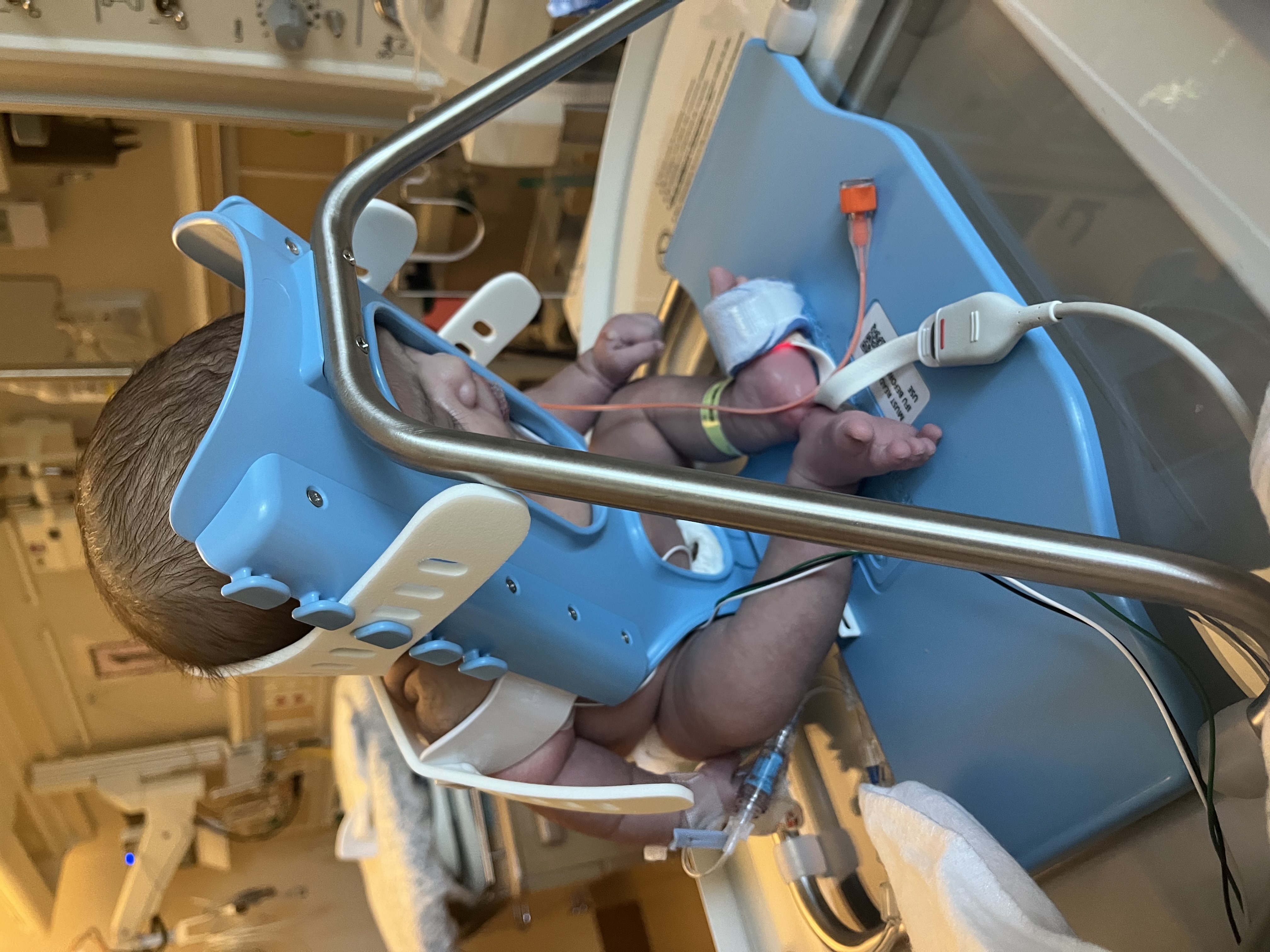
282 - To Cradle or Not to Cradle: Can the Use of a Lumbar Puncture Cradle Increase Lumbar Puncture Success Rates?
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 282.6699
Sevag Tachejian, The Hospital for Sick Children, Toronto, ON, Canada; Adrienne L. Davis, The Hospital for Sick Children, Toronto, ON, Canada; Natasha Collia, The Hospital for Sick Children, Etobicoke, ON, Canada

Natasha Collia, MD (she/her/hers)
Pediatric Emergency Staff Physician, Trauma and Simulation Lead Educator
The Hospital for Sick Children
Etobicoke, Ontario, Canada
Presenting Author(s)
Background: Lumbar puncture (LP) has low published success rates, ranging between 50-80% in the neonatal and infant population, while traumatic taps are reported in 30-50%. Proper immobilization and utilizing the sitting position have been shown to improve success rates. The use of a novel LP cradle to standardize seated positioning and obviate immobilization variability may reduce the likelihood of repeated attempts and traumatic LPs.
Objective: To determine the first-pass success rate of LPs using the cradle compared to a control group in lateral decubitus. First-pass success is defined as obtention of cerebrospinal fluid with red blood cell (RBC) count < 10,000 cells/µL on first attempt. Secondary objectives were to compare overall LP success rate for >1 attempt, and traumatic LP rate (>400 RBCs/µL) with and without the cradle.
Design/Methods: This was a single center retrospective cohort study from August 2020 to October 2024. Term and corrected preterm infants aged ≥ 37 weeks and ≤ 3 months, presenting to the emergency, and requiring an LP were identified through an EPIC report. Unstable infants, those requiring opening pressure and charts lacking an LP procedure note were excluded. Cases using the SMöLTAP LP cradle were identified first, and concurrent controls were randomly selected. A sample size of 71 per group was calculated to detect a 20% absolute increase in first-pass success rate with 80% power and a 5% two-sided alpha. All outcomes were analyzed using chi-squared tests. Logistic regression was used to control for age, weight, prematurity, acuity, physician experience, use of local anesthetics, and day/night shift.
Results: 42 infants (71 per group) were included. Mean age was 26 days (SD 20), and 57% were male. Overall, first-pass success rate in our sample was 74/142 (52%). Use of the cradle resulted in a higher first-pass success rate χ2 (1, 142) = 7.22, p=0.007, and fewer traumatic taps χ2 (1, 118) = 8.17, p=0.005. There was no difference in overall success rate, 57/71 (80%) compared to 50/71 (70%), p=0.173. Cradle use remained significantly associated with first-pass success after adjusting for age, weight, prematurity, acuity, physician experience, use of local anesthetic, or day/night shift (OR 2.23, 95% CI 1.06-4.70, p=0.036).
Conclusion(s): An LP cradle is a promising tool for improving first-pass success of LPs and decreasing traumatic tap rates. A larger prospective study is warranted to evaluate its effectiveness and potential impact on clinical practice.
SMoLTAP: Lumbar Puncture cradle