Technology 2: Telemedicine
Session: Technology 2: Telemedicine
194 - SCD Care Anywhere: Improving Access to Care for Sickle Cell Disease through Telemedicine
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 194.6470
Seethal A. Jacob, Indiana University School of Medicine, Indianapolis, IN, United States; Brenda White, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States; Jillian Bouck, Indiana University School of Medicine, Indianapolis, IN, United States; matthew aalsma, Indiana University School of Medicine, Indianapolis, IN, United States
.jpg)
Seethal A. Jacob, MD, MS (she/her/hers)
Associate Professor of Pediatrics
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Comprehensive medical care can decrease the adverse outcomes associated with Sickle Cell Disease (SCD), but this is not easily accessed. Telemedicine can potentially address barriers experienced by patients with SCD, as it can increase local access to subspecialty care, while also improving treatment adherence and decreasing patient/caregiver stress and burden.
Objective: The purpose of this study was to evaluate the feasibility and acceptability of telemedicine for the provision of pediatric SCD care in medically underserved areas of the Midwest.
Design/Methods: This is a prospective cohort study evaluating the implementation of two telemedicine models adapted for SCD: 1) Hub and Spoke; and 2) Direct-to-Consumer (DTC). Models were modified based on caregiver/patient input, including addition of a remote physical exam device to the DTC model (Figure 1). Patients were assigned to a model based on location. Self-report of telemedicine satisfaction, communication, and trust were collected, as well as process of care measures collected from the medical record.
Results: Interim results included 44 telemedicine visits for 18 enrolled subjects of varying SCD genotypes. Each patient completed an average of 2.4 virtual visits. Average patient age was 10.9 years (range 4 to 18). Average distance to the SCD subspecialty center was 155 miles. Average area deprivation index was 7.2 (Range 1-10; 10 = most disadvantaged) and average childhood opportunity index was 1.9 (Range 1-5; 1= Very Low). Over the last 12 months, 83% of visits were virtual for this cohort.
Regardless of model, caregivers reported less time lost from work/school on study than pre-study. Most caregivers reported “Excellent”/“Good” satisfaction with their model, including their comfort with the equipment, and time and thoroughness of the SCD provider (Table 1). When asked specifically about communication, caregivers were satisfied with their SCD provider. All caregivers endorsed trust of their SCD team, as well.
On average, less visits were missed (Table 2). There also was no change in prescribing of therapies or adherence to health supervision guidelines for SCD except urine protein assessments.
Conclusion(s): Disease-adapted telemedicine models are feasible and acceptable. Optimization of telemedicine can close access gaps experienced by vulnerable chronic disease populations like SCD. Further research to establish effectiveness, as well as to understand caregiver/patient perspectives on the inclusion of digital interventions such as mHealth applications into virtual care may allow expansion of comprehensive care standards for all SCD age groups.
Figure 1: SCD Care Anywhere Telemedicine Models: Hub-and-Spoke vs Direct-to-Consumer
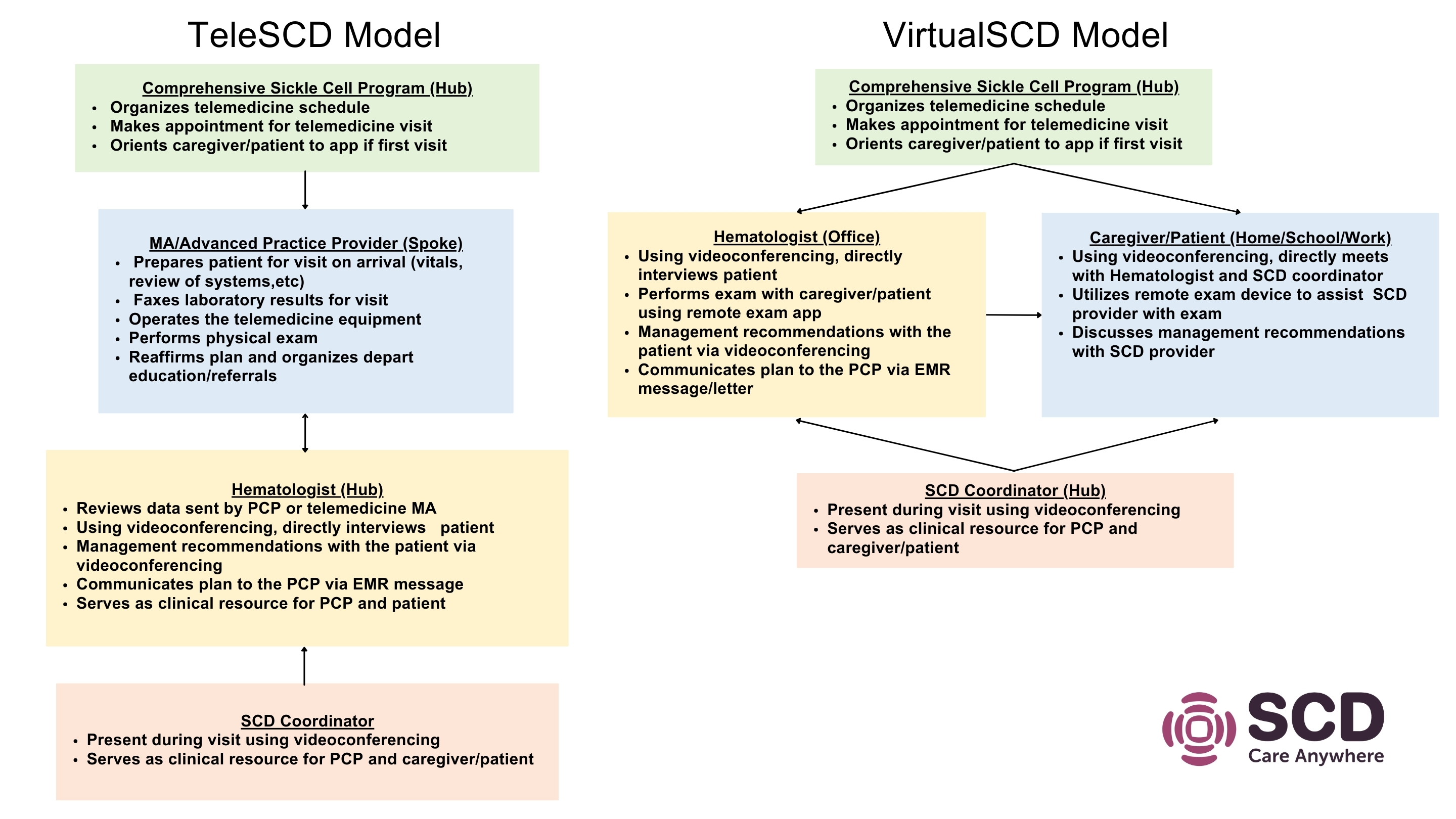 Hub-and-Spoke and Direct-to-Consumer models developed and adapted with caregiver and patient input on barriers and facilitators to telemedicine use.
Hub-and-Spoke and Direct-to-Consumer models developed and adapted with caregiver and patient input on barriers and facilitators to telemedicine use.Satisfaction with Telemedicine Services
Table 1 PAS Abstract.pdfSatisfaction as measured by the validated Telemedicine Satisfaction Survey (TeSS) completed after a virtual visit.
Table 2: Interim Results of Sickle Cell Disease Care Measures
Table 2 PAS Abstract.pdf

