Neonatal Hemodynamics and Cardiovascular Medicine 4
Session: Neonatal Hemodynamics and Cardiovascular Medicine 4
089 - Use of Vasopressin and Norepinephrine in Neonatal septic shock- A multi-center retrospective cohort study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 89.6734
Renjini Lalitha, The University of Western Ontario - Schulich School of Medicine & Dentistry, London, ON, Canada; Najlaa Abdulaziz, No, Madinah, Al Madinah, Saudi Arabia; Michael Miller, The University of Western Ontario - Schulich School of Medicine & Dentistry, London, ON, Canada; Kelly L. Mendham, London Health Sciences Centre, London, ON, Canada; Ashraf Kharrat, Mount Sinai Hospital, Toronto, ON, Canada; Gabriella Ripstein, University of Ottawa Faculty of Medicine, Toronto, ON, Canada; Sebastien Joye, centre universitaire hospitalier vaudois, Lausanne, Vaud, Switzerland; Poorva Deshpande, Mount Sinai Hospital, Toronto, ON, Canada; Michelle Baczynski, Mount Sinai Hospital, Toronto, ON, Canada; Faith Zhu, Faith Zhu, Staff Neonatologist, Mount Sinai Hospital, Toronto, Toronto, ON, Canada; Amish Jain, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Sagee Nissimov, Shamir Medical Center, Ramat Hasharon, HaMerkaz, Israel; Audrey Hebert, CHU de Quebec - Universite Laval, Quebec city, PQ, Canada; Simon Ouellet, Faculty of Medicine Université Laval, Quebec, PQ, Canada; Marie-Eve Leclerc, Faculty of Medicine Université Laval, Québec, PQ, Canada; Soume Bhattacharya, Western University, London, ON, Canada

Soume Bhattacharya, MBBS,MD (she/her/hers)
Assistant Professor
Western University
London, Ontario, Canada
Presenting Author(s)
Background: Vasopressin (VA) and norepinephrine (NE) are pressors that are increasingly being used in neonates. More recently, there has been wider application of NE in the management of neonatal warm septic shock. While biological rationale is sound given the speculation of low VA levels in septic sate, use of VA in septic shock remains underexplored in neonates.
Objective: To describe the use of VA and NE in neonates with warm septic shock, focusing on their effects on physiological indices of cardiorespiratory stability and overall outcomes across three tertiary Neonatal Intensive Care Unit (NICU) in Canada.
Design/Methods: This was a retrospective study that involved neonates with warm septic shock who received VA or NE between Jan 2015-Dec 2020 at 3 Canadian level III NICU. Receipt of both VA and NE were excluded. Data was collected from medical records on demographic information, cardiorespiratory parameters and clinical outcomes. Independent t-tests/Mann-Whitney U tests and chi-square tests/Fisher’s exact tests were used to compare groups for continuous and categorical variables, respectively; repeated measures analysis of variance was used to examine trends in physiological parameters over time between groups.
Results: 58 neonates (VA: 21, NE: 37) were included in this study. Mean gestational age (GA) and birth weight were significantly higher in VA group compared to NE group- 27.1 (4.1) in VA group and 24.9 (2.8) in NE group, p= 0.015 (Table 1). VA was used more frequently as a second line agent in 57.1%, while NE as first line agent in 62.2%, p=0.016. Notably, VA neonates had significantly higher mean FiO2 (SD) at initiation compared to NE group (71.1[34.1] Vs 47.5[24.5], p 0.026) with earlier postnatal age for its use (8.4[7.2] Vs 13.7[9.1] days, p=0.025).
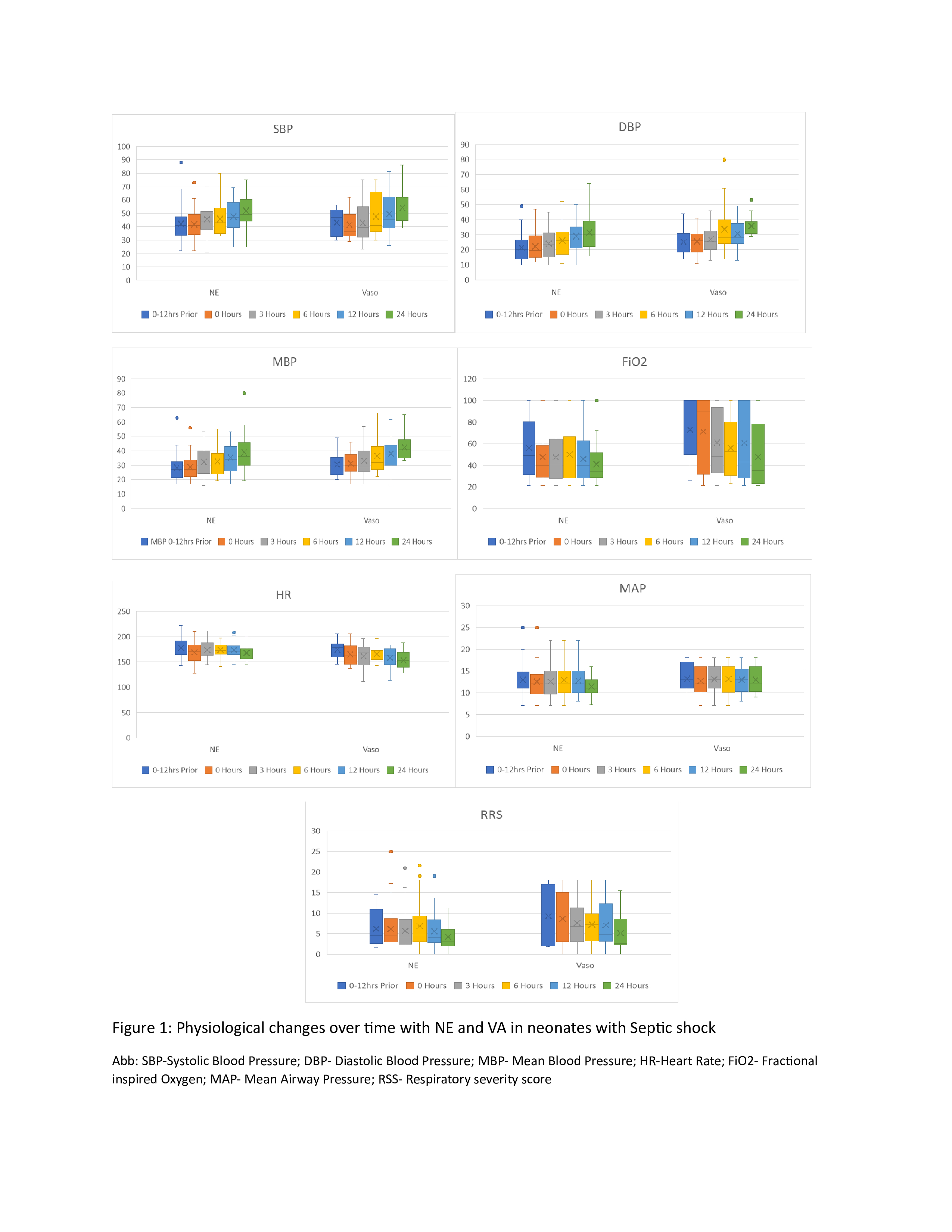
Enhancement in physiological parameters were observed over the course of treatment with both agents as shown in Figure 1, with similar treatment response to each agent. Mortality within the first 7 days of use was 38.1% (n=8) and 27% (n=10), p=0.381 in the VA and NE group, respectively. Median length of hospital stay (IQR) was significantly shorter in VA group at 21 (11-38) days compared to NE group at 56 (24-126) days. Other outcomes were comparable between groups (Table 2)
Conclusion(s): This study describes the use of VA and NE- two uniquely distinct pressors- in neonatal septic shock, providing pragmatic insights into its use. While use of VA in septic shock looks promising, further prospective studies exploring its use as first line agent in septic shock and further detailing its cardiopulmonary effects and safety profiles are warranted.
Table 1: Cohort description for Vasopressin and Norepinephrine use for septic shock
.jpg)
Table 2: Outcomes among neonates who received Vasopressin and Norepinephrine for septic shock
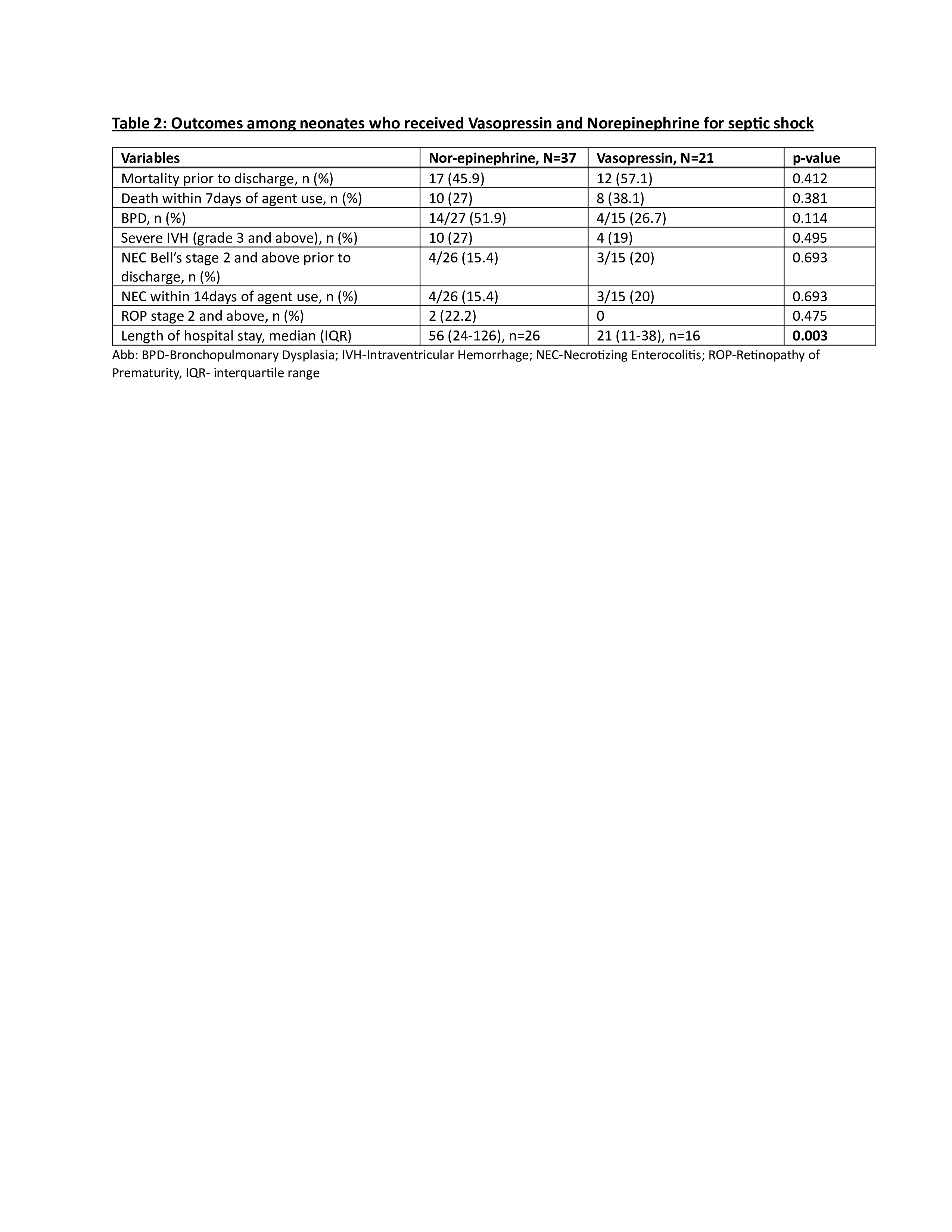
Figure 1: Physiological changes over time with NE and VA in neonates with Septic shock