Medical Education 5: Procedures and Simulation
Session: Medical Education 5: Procedures and Simulation
241 - The Acceptability, Appropriateness and Feasibility of the Implementation of a Structured Program for Pediatric Emergency Care Coordinators: A Multi-State Prospective Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 241.6952
Cage T. Cochran, Yale School of Medicine, New Haven, CT, United States; Sally K.. Snow, self employed, Graham, TX, United States; Camilia Brandt, Improving Pediatric Acute Care Through Simulation, Fenton, MI, United States; Erin Montgomery, Indiana University School of Medicine, Indianapolis, IN, United States; Benjamin Michaels, Improving Pediatric Acute Care Through Simulation (ImPACTS), Guilderland, NY, United States; Elizabeth Sanseau, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Sofia Grigoria Athanasopoulou, Yale School of Medicine, New Haven, CT, United States; Marc Auerbach, Yale School of Medicine, new haven, CT, United States

Cage T. Cochran (he/him/his)
Research Associate
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Mortality rate is four times higher when children are cared for in Emergency Departments (EDs) with low Pediatric Readiness. A 12 month program was developed and implemented with the goal of improving Pediatric Readiness. The program involved a cohort of mentors that supported Pediatric Emergency Care Coordinators (PECCs) working to achieve structured milestones in their EDs.
Objective: To describe the implementation, acceptability, appropriateness and feasibility of a PECC mentorship program in TX and MI.
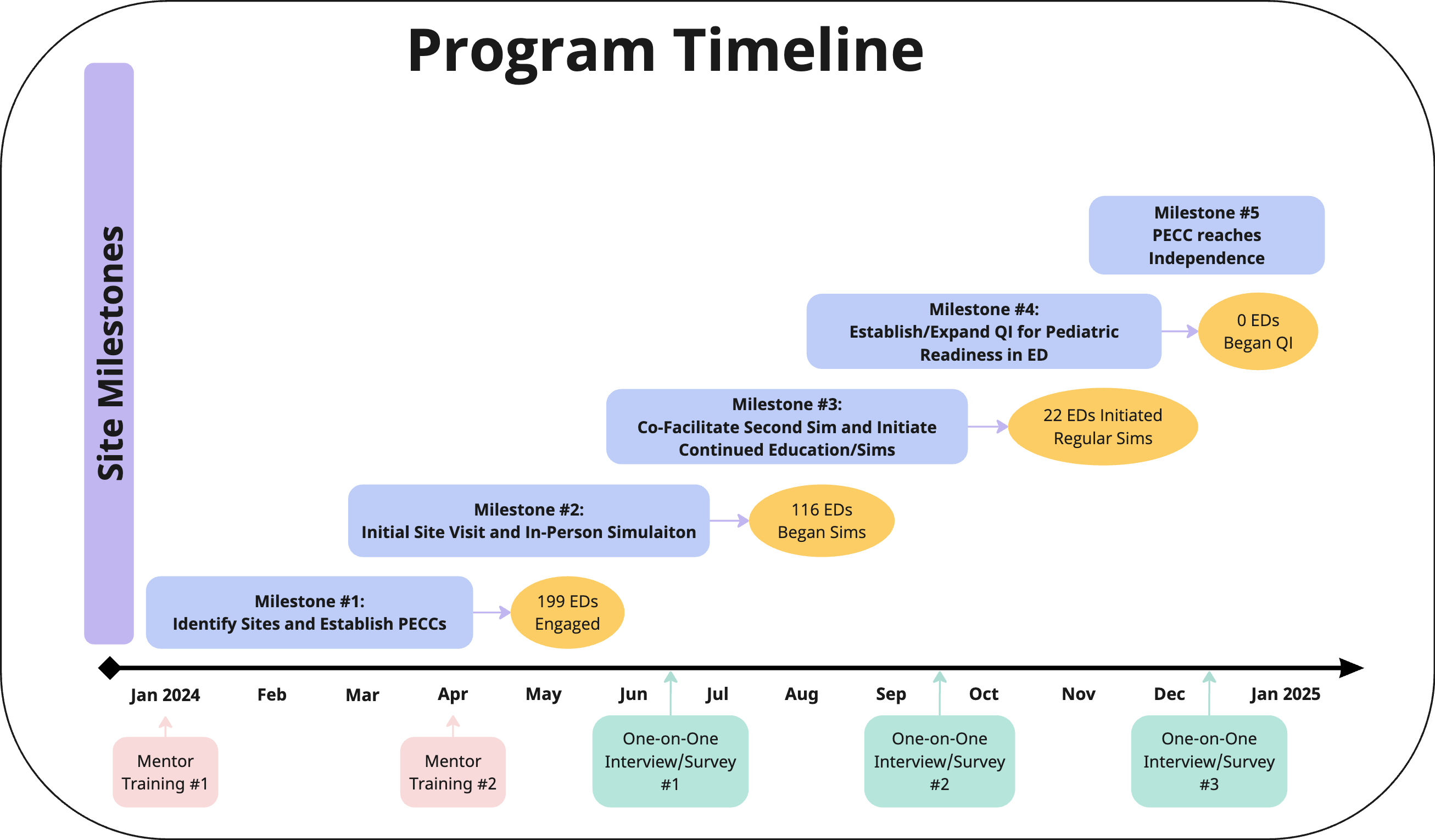
Design/Methods: Mentors were recruited through regional nursing networks in TX and MI by state-level project facilitators. Mentors were hired across geographic regions to achieve state coverage. A project manager and administrator supported all activities. To start the program, mentors completed a one-day in-person training on the structured milestones, simulation (sim) facilitation, and Pediatric Readiness. Mentors recruited at least two local EDs to participate by designating a PECC. Structured milestones were provided to the mentors and PECCs to guide their work. An online community of practice on Zulip provided ongoing support and resource sharing. The project manager held a bi-weekly check-in meeting with all mentors. Mentors completed monthly activity logs and site trackers related to the milestones. The acceptability, appropriateness, and feasibility were measured quarterly, using a twelve-question validated 5 point Likert scale tool and qualitative interviews of mentors.
Results: Thirty-six mentors engaged 199 EDs total (TX: 170, MI: 29). Thirty-four mentors (94.4%) met the goal of engaging at least 2 EDs, and the majority (58.3%) engaged at least 5 EDs. Of the EDs engaged, 116 (58.3%) had an initial sim, but only 22 sites (11.1%) initiated continual sims. No sites started quality improvement (QI) or achieved PECC independence. In total, mentors reported 282 sims and 1968 participants. Themes of the qualitative interviews included mentors requesting additional resources and strategies to achieve later milestones. The aggregated net promoter score was high at 91.8. Mentors reported high mean Likert ratings for feasibility (4.44), acceptability (4.78), and appropriateness (4.82) in all evaluations.
Conclusion(s): Mentors were successful in initial engagement and education with EDs but struggled to reach later milestones. Despite this, mentors expressed strong support for the program and satisfaction with their work. This program shows promise for scaling up to reach rural and underserved EDs across the US.
Program Timeline and Site Milestones
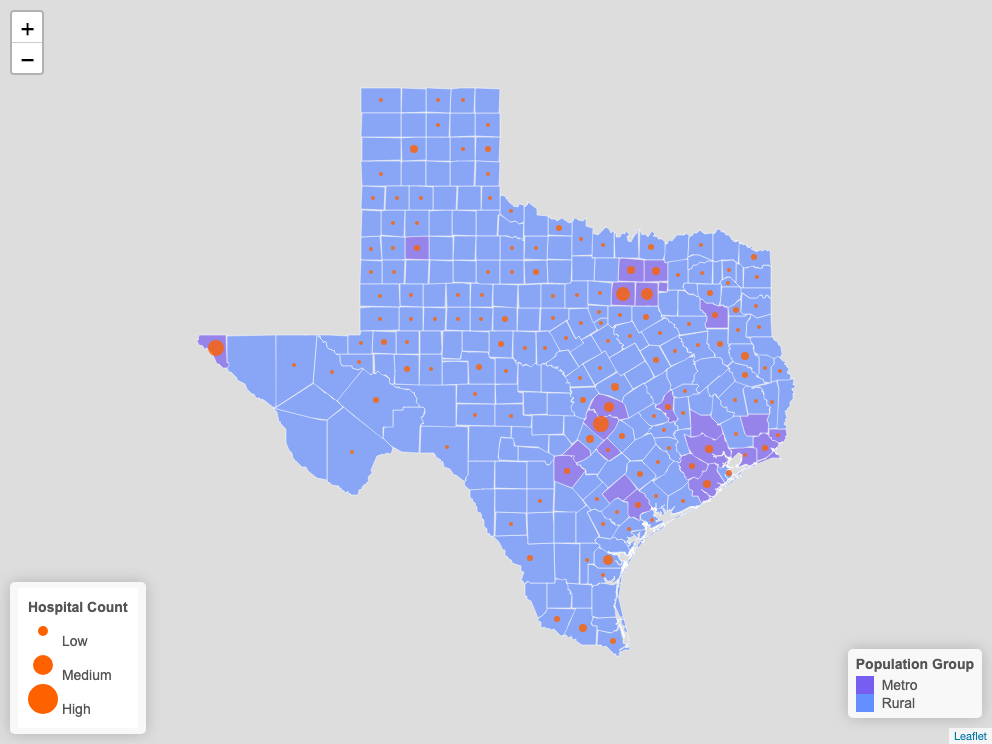
Sites Engaged in Texas
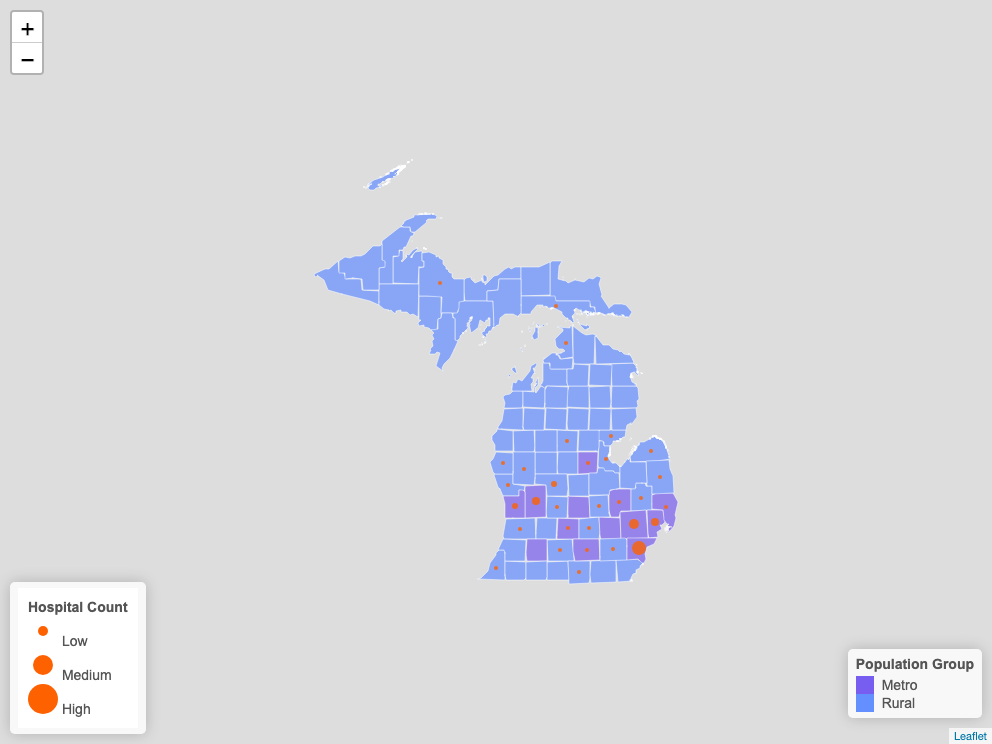
Sites Engaged in Michigan