Neonatal Hemodynamics and Cardiovascular Medicine 4
Session: Neonatal Hemodynamics and Cardiovascular Medicine 4
088 - The association between umbilical cord blood cardiac enzymes and other biomarkers of perinatal asphyxia
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 88.6915
Kathrine S. Hansen, Oslo University Hospital, University of Oslo, Tårnåsen, Akershus, Norway; Arild Rønnestad, University of Oslo, Oslo, Oslo, Norway; Anne Lee Solevåg, Oslo University Hospital, Oslo, Oslo, Norway; Ingeborg Martinsen. Østen, Institute for clinical medicine, Faculty of medicine, University of Oslo, Norway, Oslo, Oslo, Norway
.jpg)
Kathrine S. Hansen, MScN (she/her/hers)
PhD.-Student
Oslo University Hospital, University of Oslo
Tårnåsen, Akershus, Norway
Presenting Author(s)
Background: Perinatal asphyxia results in a combined respiratory and metabolic acidosis in the fetus and/or infant with a risk of damage to vital organs. Currently diagnostic methods for asphyxia have limited sensitivity and specificity. While the primary concern is poor neurological outcome, 25-50% of severely asphyxiated infants experience myocardial ischemia and necrosis. Troponin T(TnT) and Troponin I(TnI) are used to diagnose myocardial ischemia in adults, where the I isoform is considered more cardiac specific. Both TnT and TnI are elevated in umbilical cord blood of asphyxiated infants. However, the prognostic value of one over the other is uncertain as their reference ranges and trajectories are different. Different hospitals often analyze only one isoform.
Objective: This study aimed was to investigate how TnT and TnI are associated with each other and Apgar score and umbilical cord blood pH, lactate and other cardiac biomarkers.
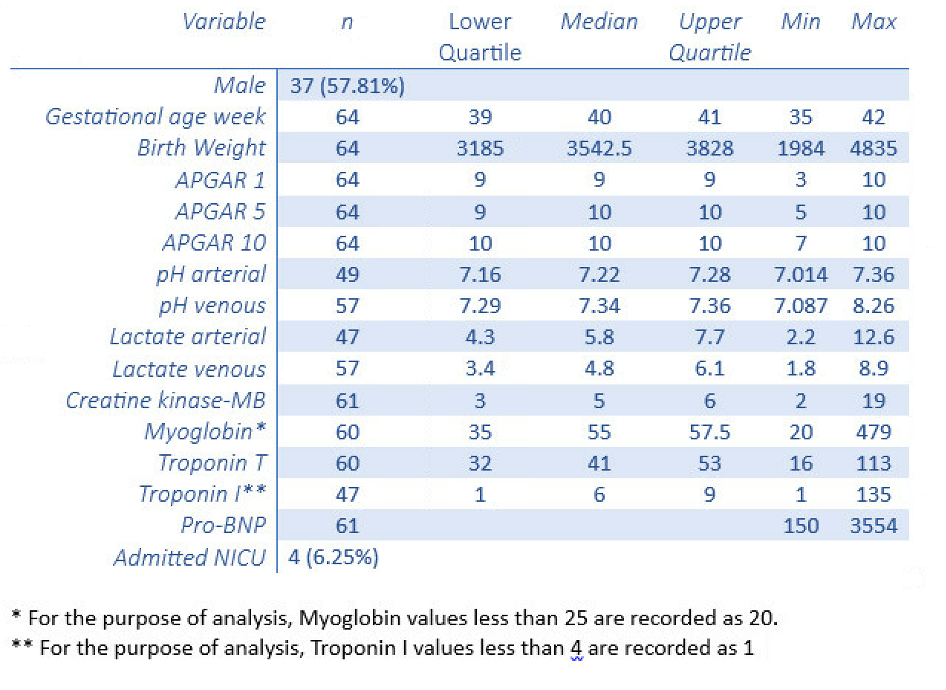
Design/Methods: This study is a clinical observational study at Oslo University Hospital (OUH), Rikshospitalet, Norway. Infants with a gestation age>36 weeks are eligible for inclusion. We collect venous umbilical cord blood samples to analyze pH and lactate, pro-Brain Natriuretic Peptide (pro-BNP), Creatine kinase-MB, Myoglobin and TnT (Dpt. of clinical biochemistry, OUH) and TnI (Dpt. Of Clinical Biochemistry, Vestre Viken Hospital). Spearman correlations were calculated for Apgar score and umbilical cord blood variables. To analyze the differences in biomarkers between infants admitted to the NICU and those who were not, we used the Mann-Whitney U test.
Results: We included 64 infants with predominantly high Apgar scores (Table 1). We did not find a significant correlation between the biomarkers, other than Myoglobin had a significant negative correlation with pH (r=-0,32, p=0,034). Arterial Lactate had a significant negative correlation with 1 minute Apgar score (r=-0,26, p=0,016). There was no difference in any biomarker between infants admitted to the NICU (n=4) and those who were not admitted (n=60).
Conclusion(s): There was no significant correlation between Troponin T and I level, or with other cardiac biomarkers in umbilical cord blood. The results indicate that lactate might be the best biomarker of mild neonatal compromise as signified by Apgar score. Considering the small and predominantly healthy population, as well as the timing of Troponin T and I sampling, we aim to continue investigating these variables in a larger population with more compromised infants.
Tabel 1